German researchers have shown that high-quality MRI scans of the shoulder can be acquired in 25 minutes at 7 tesla, making the technique clinically feasible and a realistic alternative to arthroscopy and 1.5-tesla MRI.
"While the FDA [U.S. Food and Drug Administration] has already cleared MR imaging of the knee joint at 7T as a clinical application for the latest generation of 7T MR systems, MRI of the shoulder at 7T is still in its infancy," noted Oliver Kraff, PhD, a staff scientist at the Erwin L. Hahn Institute for MRI at the University Duisburg-Essen in Essen, and colleagues.
The group used an 8-channel transmit/15-channel receive radiofrequency (RF) coil setup to evaluate eight patients presenting with shoulder pain. They presented their findings in an e-poster at the recent International Society for Magnetic Resonance in Medicine (ISMRM) annual meeting in Montreal.
RF coil setup
A previous study conducted at Essen used a two-array RF coil setup for shoulder imaging featuring an 8-channel transmit/receive coil based on microstrip lines with meanders and a 7-channel receive-only coil based on loops (Medical Physics, December 2017, Vol. 44:12, pp. 6195-6208). Anatomical images in healthy volunteers demonstrated the high performance of the RF coil setup to acquire high-resolution 7-tesla shoulder imaging with excellent image quality.
The new study presented at ISMRM 2019 included eight patients (6 men, 2 women; 48.3 ± 10.0 years) who presented with shoulder pain and were scheduled for arthroscopic surgery of the affected shoulder in the orthopedic outpatient department. Kraff's team used a whole-body research system (Magnetom 7-tesla, Siemens Healthineers) equipped with the same RF coil setup as the 2017 Essen study.
To minimize B1+ inhomogeneities while obtaining maximum signal amplitude, they used phase-only RF shimming. In total, 10 optimized sequences were included in the protocol, balancing a maximum of variety for evaluation and short examination time, the authors explained.
Details about the sequence parameters are below.
| Parameters of the 7-tesla shoulder protocol | ||||||
| Sequence & orientation | TR (msec) | TE (msec) | nom. FA (deg) | Acquired resolution (mm3) | No. slices | TA (min:sec) |
| PD TSE fs coronal | 4350 | 30 | 180 | 0.43 x 0.43 x 2.5 | 23 | 4:05 |
| PD TSE fs transverse | 4350 | 30 | 180 | 0.43 x 0.43 x 2.5 | 30 | 4:05 |
| PD TSE sagittal | 4500 | 35 | 180 | 0.40 x 0.40 x 2.5 | 30 | 3:38 |
| PD TSE coronal | 4500 | 35 | 180 | 0.40 x 0.40 x 2.5 | 30 | 3:15 |
| DESS we coronal | 8.0 | 2.4 | 15 | 0.70 x 0.70 x 0.70 | 128 | 4:56 |
| T1 TSE coronal | 900 | 11 | 180 | 0.40 x 0.40 x 2.5 | 9 | 1:43 |
| T1 GRE sagittal | 172 | 4.1 | 70 | 0.45 x 0.35 x 2.0 | 40 | 5:24 |
| T1 GRE coronal | 172 | 4.1 | 70 | 0.45 x 0.35 x 2.0 | 40 | 5:24 |
| MEDIC coronal | 1000 | 15 | 30 | 0.35 x 0.35 x 1.5 | 39 | 5:21 |
| STIR coronal | 4500 | 31 | 180 | 0.70 x 0.70 x 3.0 | 20 | 1:59 |
Two radiologists separately assessed image quality for each patient and each sequence. The presence of artifacts was rated on a five-point scale, the effect of B1+ inhomogenities on a three-point scale, and the delineation of anatomical structures on a four-point scale. The higher ratings indicated better image quality.
The same radiologists generated in consensus a structured report focusing on the rotator cuff, assessing fatty atrophy of the rotator cuff muscles, supraspinatus atrophy, the subacromial subdeltoideal bursa, lesions of the tendons, degeneration of acromioclavicular joint, effusion of the glenohumeral joint, the status of the cartilage, and the labrum.
The report was then compared with the report from arthroscopy, regarded as the gold standard. Pathologies found at 7-tesla MRI were visually compared with preexisting 1.5-tesla MR images from the same patients.
What was the outcome?
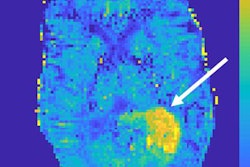
The researchers found very good image quality with hardly definable artifacts in proton density (PD)-weighted turbo spin-echo (TSE) fat-saturated sequences, plus moderate artifacts in multiple-echo data image combination (MEDIC) and short tau inversion-recovery (STIR) sequences. They found the most homogeneous B1+ field in T1-weighted gradient-recalled echo (GRE) and double-echo steady state (DESS) sequences. Strongest inhomogeneities appeared in MEDIC coronal and proton density TSE sagittal imagees.
With the exception of vessels and nerves, the delineation of anatomic structures was best in PD TSE fat-saturated sequences and impaired in MEDIC and STIR sequences. For vessels and nerves, PD TSE coronal and T1-weighted GRE sequences were rated best, while fat-saturated PD TSE sequences underperformed. For evaluating muscle tissue, DESS and T1-weighted GRE could complement proton density-weighted TSE fat-saturated sequences, the researchers noted.
Rotator cuff pathologies were identified at 7 tesla in all patients. Correlated with the arthroscopical report (delay between 7-tesla MRI and arthroscopy was two to 15 days in seven patients and 70 days in one patient), pathologies of the rotator cuff tendons were widely overdiagnosed with 7-tesla MRI, the group found.
Arthroscopy confirmed tendinitis or partial tear of the supraspinatus tendon in only three of the eight patients and of the subscapularis tendon in one of the six patients. It missed tendinitis or partial tear of the infraspinatus tendon in one patient.
Only one pathology of the rotator cuff, a partial lesion of the subscapularis tendon, was missed with 7-tesla MRI. Pathologies of the long bicipital tendon, the acromioclavicular joint, the glenohumeral cartilage, the labrum, and the subacromial subdeltoideal bursa were mainly concordant with both arthroscopy and 7-tesla MRI. Exceptions were one lesion of the long bicipital tendon, one subacromial bursitis, and one superior labral tear from anterior to posterior (SLAP) lesion missed at 7 tesla.
Preexisting 1.5-tesla MR images could be collected from three patients, with the delay between the two exams being 34, 34, and 49 days, respectively. The main pathologies were visible at both field strengths, but pathologies were more distinct at 7 tesla due to better contrast and higher image resolution, according to the researchers.
"Feasibility of clinical 7T MRI of the shoulder was demonstrated," noted Kraff and colleagues from the department of diagnostic and interventional radiology and neuroradiology, the department of trauma and orthopedic surgery, and the High Field and Hybrid MRI Center at University Hospital Essen and the Facharztklinik Essen.
"A comprehensive protocol should include fat-saturated PD TSE sequences (excellent delineation of almost all anatomical structures) in axial and coronal orientation and a DESS sequence (isotropic high resolution and muscle delineation)," the researchers added.
A T1-weighted GRE sequence with its good depiction of vessels and nerves may complement the protocol, while the use of STIR needs to be postponed until substantial optimization yields better results, they noted. Overall, this comprehensive protocol results in a clinically relevant total acquisition time of 25 minutes, the authors concluded.