There are many new applications for imaging data, and radiologists need to jump in to make themselves future-proof, according to Dr. Peter van Ooijen, an associate professor of medical imaging informatics at the University Medical Centre Groningen in the Netherlands. Technologies for 3D visualization are rapidly gaining importance, and to guarantee their future survival, radiologists must understand their potential, as well as their pitfalls.
Among the applications of 3D imaging are preplanning surgical procedures. In surgical planning, other physicians in the hospital need to use radiological data, so the data must be suitable for more than simply your own diagnosis, van Ooijen pointed out.
With 3D imaging, radiologists can print 3D models of tissue or bones that surgeons can hold physically in their hands to gain additional insight or to practice upon. Such models can also be used for anatomical education because they show a wider variety of pathologies than students would see in a book, he said.
Radiologists can create virtual reality (VR) environments where surgeons can practice before surgery, while augmented reality (AR) overlays can give advanced support during the procedure itself. In addition, radiology is moving from describing images toward making measurements, and that includes measuring in 3D, van Ooijen explained.
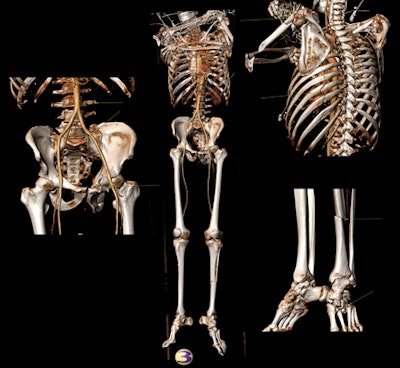
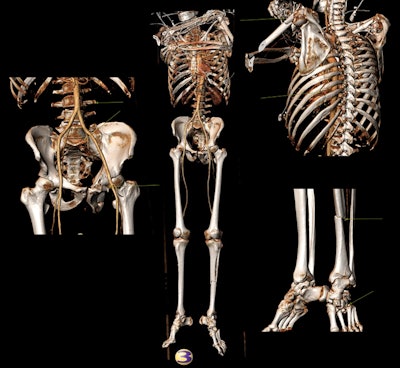
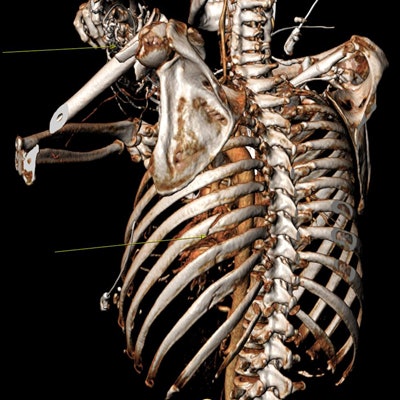
A trauma patient with multiple fractures underwent a whole-body CT scan. The 3D images clearly depicted the fractures (yellow arrows) and allowed them to be classified. Images provided by Dr. Thomas Frauenfelder.
Many pitfalls of 3D visualization arise from the flexibility and versatility of software packages, he noted. By providing a wide range of options for segmentation and visualization, they can increase the risk of making mistakes. Furthermore, the acquired imaging data may not be right for the application that the radiologist intends -- e.g., where the settings for a CT scan aren't appropriate for a subsequent, more comprehensive, 3D workup.
"If you use an automated bone removal tool for 3D rendering of the internal carotid artery, it's easy for important structures, which should be there, to be deleted. This can lead to an incorrect interpretation and diagnosis, and have an adverse influence on therapy," said Dr. Thomas Frauenfelder, a professor of radiology and vice director of the Institute of Diagnostic Radiology at the University Hospital of Zurich, who is speaking at the same session.
Frauenfelder will discuss how semiautomated 3D postprocessing can bring additional value to lung, cardiovascular, and bone imaging, including detecting lung nodules and imaging lung structure and bone fractures. With a volume rendering of a pelvic fracture, you can get an overview of the entire situation, rather than having to scroll through multiple images of individual fracture lines, he stated.
Radiologists often don't have the passion or time to make a colored 3D rendering or other special image displaying the whole pathology, which would be attractive to attending physicians and potentially to patients, he said.
To help free up time for 3D imaging, Frauenfelder recommends having a clear diagnostic workflow. This is important because no one will use it if it's too time-consuming, he said.
At Zurich, all radiologists are expected to use 3D imaging, and to save time, oblique multiplanar reformatted (MPR) images are provided automatically by the software. The same cloud- or server-based software is used through the entire institute, again to ensure that workflow is centralized and time savings are maximized.
For van Ooijen, getting radiologists to adopt visualization, processing, VR, and AR technologies is all about training. Imaging informatics and its new technologies should be an integral part of training to help people deal with these technologies, but they're not fully integrated everywhere, he said. Special training is needed because of the sheer speed of development of visualization and processing technologies.
As a board member of the European Society of Medical Imaging Informatics (EuSoMII), van Ooijen is trying to set up a framework on a European level to incorporate new technologies, such as 3D printing and AR, into radiology training. Within individual countries, he's exploring the possibility of both training radiologists in a specific disease type or body part and giving them a specialization in imaging informatics. This, he believes, would help them employ the new technology in their department in the most appropriate way.
Originally published in ECR Today on 28 February 2018.
Copyright © 2018 European Society of Radiology



















