VIENNA - A fully automated algorithm to evaluate airway disease produced good to excellent results from MDCT images, according to a presentation this week at ECR 2016.
The group from Heidelberg, Germany, developed a lobe-based lung segmentation algorithm and applied it to volumetric inspiratory and expiratory CT scans of children with cystic fibrosis. Overlap with manually generated masks reached 97% for the inspiratory scans and 90% for expiratory scans, depending on the reconstruction kernel, offering a promising new way to quantify airway disease.
 Oliver Weinheimer, PhD, from the University of Heidelberg.
Oliver Weinheimer, PhD, from the University of Heidelberg."The new lobe segmentation system delivers excellent results for inspiratory scans and very good results on expiratory scans," said Oliver Weinheimer, PhD, from the University of Heidelberg. "It can be an important component for lobe-based computation of airway diseases such as cystic fibrosis or chronic obstructive pulmonary disease [COPD], and could reduce the necessity for user interaction in lung MDCT postprocessing."
Lobe-based analysis of the airways and lung parenchyma presents important opportunities to describe the severity of airway disease, either at a single time point or over a period of time, Weinheimer said. In the case of COPD, for example, it's important to know where the emphysema is located. Quantification of emphysema can be done on inspiratory scans.
In the case of cystic fibrosis, it's important to know where it is located as well. Cystic fibrosis can be quantified on expiratory scans. CT shows that these diseases are not distributed evenly over the lungs, and there are differences in the different lobes.
"What is needed is an accurate lobe segmentation algorithm," Weinheimer said. "It should work on both inspiratory and expiratory scans, and it should be validated."
The study used spirometry-controlled, matched inspiratory and expiratory low-dose CT scans from 16 schoolchildren (11 ± 2.4 years of age) with cystic fibrosis. CT scans were acquired for each patient at four time points: at baseline, three months, one year, and two years, at 100 kVp and 30 mAs to 50 mAs. The images were reconstructed using soft (B30f) and harder (B60f) kernels to aid in the analysis. Spacing was at 0.46 mm to 0.78 mm for the 0.6-mm slices. Pitch was set at 1 for inspiratory scans and at 1.2 for expiratory scans, resulting in 256 MDCT volumes.
Under the hood: The algorithm
The lobe segmentations were performed with a self-adapting, iterative, region-growing algorithm. First, the CT images were skeletonized using a topology-preserving, 3D thinning algorithm, and the skeleton was then transformed into an acrylic graph representation. The airways were labeled using a rules-based method that allowed for anatomic variation, Weinheimer said.
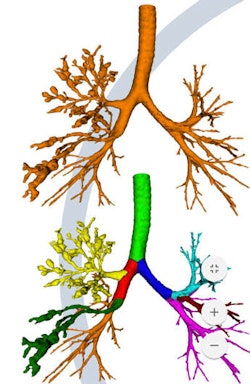 Airway segmentation with vessels assigned to each lobe. Image courtesy of Oliver Weinheimer, PhD.
Airway segmentation with vessels assigned to each lobe. Image courtesy of Oliver Weinheimer, PhD.The team used threshold-based segmentation to segment the vessels, with adjusted thresholds for each scan, and 3D connected vessel objects were then generated from the data, he said. A convex hull of segmented bronchi is used to assign vessels to the correct lobe.
"If a vessel object is not assignable [to a lung lobe], then it is divided into smaller vessel objects" via an erosion algorithm, "and at the next iteration step the algorithm tries to find the correct lobe," Weinheimer explained. Fissures are enhanced via a Hessian matrix approach applied to the CT data.
Finally, lobe masks "are generated by distance measure to the labeled bronchi and vessels," he said. The lobe masks are then eroded, and the enhanced fissure information was used as input for a watershed transformation to fill gaps in the images.
The researchers compared manual lobe segmentation by an experienced radiologist with the fully automated technique, calculating the overlap between the two.
"What we found is that the algorithm works best on inspiratory scans," Weinheimer said.
Based on Dice index calculations, the average overlap for inspiratory scans including all lobes and time points was 97.5% ± 1.5% for the soft-kernel reconstruction and 96.4% ± 7.4% for the hard kernel. For expiratory scans, the average overlap was 86% ± 12.6% for the soft kernel and 90.1% ± 8.5% for the hard kernel.
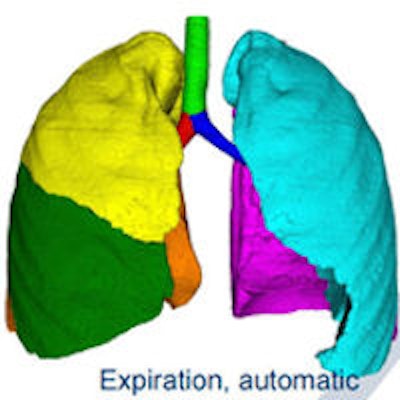
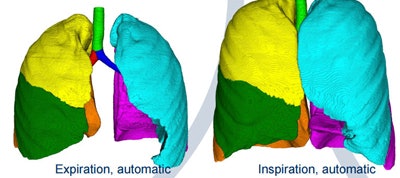 Final automated segmentation result with lobe masks generated by distance measured to labeled bronchi and vessels, with expiration at left and inspiration at right. Image courtesy of Oliver Weinheimer, PhD.
Final automated segmentation result with lobe masks generated by distance measured to labeled bronchi and vessels, with expiration at left and inspiration at right. Image courtesy of Oliver Weinheimer, PhD.The right lower lobe saw the best overlap results at 98.3%; the right middle lobe expiratory scans were the worst at 74.9%. Overlap was not influenced by the time point of the four scans -- in fact, none of the time point differences were significant.
Results were excellent for inspiratory scans and good for expiratory scans, Weinheimer concluded.
The algorithm "can be an important component for lobe-based computation of airway diseases ... and the automatic approach will reduce the necessity for user interaction in MDCT postprocessing," he said.
Another important advantage is that automated segmentation is calculated in a couple of minutes, compared with more than an hour for the manual technique, offering the potential to incorporate the information it provides routinely in the diagnosis of patients with airway disease.



















