VIENNA - Even dialysis patients can safely undergo contrast-enhanced MRI without the risk of nephrogenic systemic fibrosis (NSF) if a few safety guidelines regarding dose and contrast type are followed, according to the final results of the multicenter Pro-FINEST study presented on Sunday at the European Congress of Radiology (ECR).
In more than 500 patients exposed to the agents since 2009, French researchers found a few skin lesions but not a single case of NSF, leading them to conclude that modern contrast agents in reasonable doses can all but eliminate the risk of NSF, even among the most vulnerable patients.
"If you follow the recommendations properly, you probably won't see NSF," said Dr. Sabine Amet, from Pitié-Salpêtrière Hospital, in her presentation.
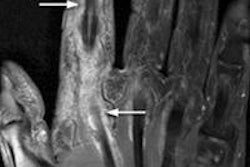
Nephrogenic systemic fibrosis -- a cutaneous and systemic disorder characterized by widespread tissue fibrosis -- has been tied to the use of gadolinium-based contrast agents (GBCAs), especially in dialysis patients. First identified in San Francisco in 2000, incidence of the sometimes fatal condition peaked in the mid-2000s but has diminished to the point of nearly disappearing in recent years.
The French national Pro-FINEST (Etude Prospective sur la Fibrose Nephrogenique Systemique) study, begun in 2008, is endorsed by the French Health Products Safety Agency (Afssaps) and the French Societies of Nephrology, Dermatology, and Radiology, Amet said. Investigators in nine French nephrology departments aimed to determine the prevalence of NSF after an MRI exam with or without gadolinium-based contrast in dialysis patients, mostly stage IV. The initial results were presented at the 2011 European Congress of Radiology, with final results of the retrospective study presented on Sunday.
The study was based on a three-section patient form, with section 1 covering demographics and dialysis, section 2 covering the MRI exam, and section 3 addressing any dermatological event. "If there is a case of NSF, the second part of the study is to perform an ancillary study to evaluate risk factors in NSF-affected patients," Amet said, and if not, no further data were to be collected.
Beginning in 2009, the researchers enrolled 571 patients with a mean age of 63.3 years, including 58.4% men. A total of 443 forms were received; they indicated that 56% of patients received gadolinium-based contrast agents, with 89.9% (n = 255) of 287 injected patients received gadoterate. Others received gadobenate (n = 12), gadobutrol (n = 11), gadopentate (n = 5), gadoteridol (n = 2), and gadodiamide (n = 1).
Doses ranged from 0.1 to 0.3 mmol/kg, but 75.9% of patients received doses less than 0.3 mmol/kg, Amet said. Fourteen MRI scans were cancelled for various reasons. Fifty patients (8.8%) were deemed lost to follow-up due to missing data, she said. The main causes of end-stage renal disease were the same as in the general population.
"Twenty-two patients reported skin lesions -- about 4% of all patients -- including about 5% of injected patients and 3% of noninjected patients," Amet said. "To conclude, we have noticed no case of NSF in 571 patients."
As for guidelines, the French drug agency and, recently, the U.S. Food and Drug Administration (September 2010) have contraindicated the use of high-risk gadolinium-based contrast agents (gadodiamide and gadopentate dimeglumine) in patients with a glomerular filtration rate less than 30 mL/min/1.73 m2, Amet said.
In these patients, the agencies recommend the lowest possible dose of moderate-risk gadolinium-based agents (gadobenate dimeglumine), or low-risk agents including gadobutrol, gadoteridol, or gadoterate.
Following the guidelines will all but eliminate the risk of NSF "even in patients at risk of NSF," Amet said.