VIENNA - Breast cancer is the most common carcinoma in women worldwide and a leading cause of death. Standardized therapy protocols aimed at maximizing the rate of breast conserving treatment and the emergence of breast units facilitate treatment while ensuring high-quality patient care. All imaging modalities play a role in the detection and characterization of the disease, including breast MRI, which has undergone a careful evidence-based evaluation and is now increasingly used in clinical practice. Professor Francesco Sardanelli, director of radiology at the IRCCS Policlinico San Donato in Milan, Italy, will focus on evidence-based controversies in breast MRI during a dedicated course today at the congress; he told ECR Today more about it ...
ECR Today: What is MR's main advantage over other modalities in both screening and staging breast cancer?
 Francesco Sardanelli is a radiologist at IRCCS Policlinico San Donato in Milan and professor of radiology at the University of Milan School of Medicine, Italy.
Francesco Sardanelli is a radiologist at IRCCS Policlinico San Donato in Milan and professor of radiology at the University of Milan School of Medicine, Italy.
Francesco Sardanelli: The main advantage of breast MRI, in screening, is higher sensitivity. In a high-risk population, the sensitivity of MRI is over 90% whereas that of mammography plus ultrasound is 60% to 65% at best. The same is true for local staging concerning the diagnosis of multifocal, multicentric, and synchronous bilateral cancers.
ECRT: How high is the percentage of high-risk women compared to the total breast cancer population?
FS: In general, in developed countries, we estimate that 5% of cancers are clustered in families with a genetic predisposition to this disease. Half of them are due to BRCA1 or BRCA mutations (and a small fraction to P53 mutations), and the other half to other genes or combinations of genetic mutations, which are still unknown and which won't be easy to identify any time in the near future. Another small but clinically significant group of women at high risk of breast cancer are those who have been treated with mantle radiation therapy (typically for Hodgkin's lymphoma), between 8 and 30 years of age. They should also have annual breast MRI screening.
ECRT: Are all high-risk women screened once a year with breast MRI? If not, should they be?
FS: Yes, they should be screened with MRI. Only a fraction of them are included in dedicated b-MRI screening programs today. It is very hard to say what the percentage is in European countries right now, but I suspect it's low.
ECRT: What are the controversies surrounding the use of breast MRI in screening this population?
FS: On this topic, the controversy is now quite limited. There is a general agreement on this issue due to a large body of evidence already published in the literature, as shown by the recommendations already issued, not only byour European Society of Breast Imaging (EUSOBI) but also by the European Society of Breast Cancer Specialists (EUSOMA), the American Cancer Society (ACS), the National Institute for Clinical Excellence (NICE), and other bodies. The discussion now is about the possibility of moving from the old paradigm of ‘MRI as an adjunct' to the new one, ‘MRI alone.' This possibility has been clearly demonstrated by two recent European studies, the German EVA trial and the Italian HIBCRIT-1 trial. If a breast MRI screening is negative, the added diagnostic value of mammography and US is not significant, as shown in figure 1.
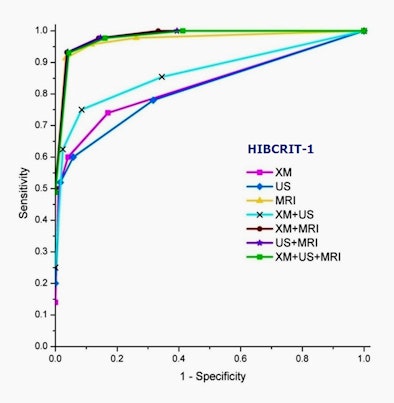 |
| Figure 1: Receiver operator characteristics (ROC) analysis of diagnostic performance of mammography (XM), ultrasonography (US), and MRI for 1,592 screening events in 501 high-risk women studied in the Italian HIBCRIT-1 study. During the study 52 breast cancers were found; 48 were screen detected and three were interval cancers. No significant differences in the area under the curve were found between MRI alone and MRI plus XM and/or US, showing that if screening MRI is negative, conventional imaging does not add any diagnostic power. (Provided by Prof. Francesco Sardanelli) |
ECRT: How high should the risk level be in order to justify annual contrast-enhanced breast MRI screening?
FS: The lifetime risk which justifies annual MRI is a lifetime risk equal to or greater than 20%, while the average lifetime risk is about 10%. However, methods for calculating individual risk are not that good, especially when risk is not very high. This remains a problem that needs to be solved.
ECRT: What is the value of contrast-enhanced breast MRI over unenhanced breast MRI and in which case should we use contrast enhancement?
FS: For cancer screening, the current evidence is that one should always inject contrast material. Noncontrast MRI (using dedicated sequences) should only be used for the evaluation of breast implant integrity. New approaches, especially those including diffusion-weighted imaging and diffusion tensor imaging, are under investigation and may change the whole scenario in the next few years.
ECRT: What are the current controversies in the other clinical applications of breast MRI, for instance concerning treatment response to neoadjuvant chemotherapy?
FS: Breast MRI is the best imaging modality for evaluating treatment response to neoadjuvant chemotherapy (NAC), for both the early prediction of NAC effect and final presurgical definition of residual tumor before surgery. We lack randomized trials demonstrating the impact on patient outcome, but evidence of this from nonrandomized studies is already available. If we meta-analyze more than 40 studies for the ability to detect residual tumor after NAC, we obtain an area under the curve at ROC analysis over 0.85.
ECRT: What were the conclusions of the COMICE and MONET randomized trials? In which centers and patients were they carried out?
FS: COMICE is a U.K. study which failed to show significant differences in the in reincision rate in favor of preoperative MRI. Its main limitations were too many centers with little experience of breast MRI and no standardized use of MR-guidance for needle biopsy and presurgical localization. MONET is a Dutch study enrolling patients with nonpalpable lesions including benign and malignant cases, with a very high percentage of DCIS and cluster of microcalcifications. As a matter of fact, using a 3T machine, they had a sensitivity for the index cancer equal to 85%, when the meta-analysis by Peters et al (Radiology 2008), including 44 studies (many of which were old studies with outdated technology), told us that breast MRI sensitivity is 90% (and a specificity of 72%).
ECRT: What are the potential consequences of overdiagnosis and overtreatment with breast MRI? How heavy can the burden be on healthcare systems and what about the additional, unnecessary stress to patients?
FS: The potential drawback is too many mastectomies due to MRI in the staging setting.
In expert hands, this burden is quite limited or sometimes totally annulled and counteracted. There are indications, such as invasive lobular cancer, for which pretreatment breast MRI has been demonstrated to reduce the mastectomy rate. The same could be true for the NAC setting if surgeons would only trust MRI.
Preoperative breast MRI should not delay the treatment for more than one month. Moreover, women should be clearly informed of the potential risks and benefits of preoperative MRI.
ECRT: What should radiologists keep in mind in order to avoid overtreatment in breast MRI?
FS: First, they should be experts at using second-look ultrasound. They should have the option of using MR-guidance when necessary. Finally, they should ensure clear communication with the surgeon in order to be sure that they make best possible use of the information obtained from the breast MRI.
ECRT: Many countries still lack proper MR equipment. There is also a problem of standardization for many MR applications. How do these problems affect the routine use of breast MRI?
FS: The problem is that MRI units are commonly used for clinical indications with limited evidence of benefit for the patient (e.g., MRI of the spine). These units are usually located outside breast cancer centers. There are clear guidelines for technical requirements for breast MRI: see Kuhl, Radiology 2007; Mann, Eur Radiol 2008.
For further information:
Sardanelli F, Boetes C, Borisch B, et al. Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. Eur J Cancer 2010;46:1296-316.
Sardanelli F. Additional findings at preoperative MRI: a simple golden rule for a complex problem? Breast Cancer Res Treat 2010;124:717-21.
Sardanelli F. Overview of the role of pre-operative breast MRI in the absence of evidence on patient outcomes. Breast. 2010 Feb;19(1):3-6.
Sardanelli F, Podo F, Santoro F, et al. Multicenter surveillance of women at high genetic breast cancer risk using mammography, ultrasonography, and contrast-enhanced magnetic resonance imaging (the high breast cancer risk italian 1 study): final results. Invest Radiol. 2011;46:94-105.
Originally published in ECR Today March 2, 2012.
Copyright © 2012 European Society of Radiology