VIENNA - Mistakes that have an impact on patient management often stem from problems of perception, and lack of background clinical information is frequently due to communication issues, delegates heard at Saturday's packed Special Focus Session.
Good judgment comes from experience, but experience comes from bad judgment, speakers agreed, while emphasizing that radiologists can arm themselves against potential pitfalls with methods to identify and minimize danger areas. When errors do slip through the cracks, doctors should retrospectively use them for education to avoid the same mistake. Keeping personal and institutional records, as well as holding regular error meetings with obligatory attendance, is one way to learn.
"The surroundings must allow for critical appraisal and constructive debate, not dispute. Reviews are an obligatory quality control tool to show where we need improvement, and where we are good," said Dr. Cornelia Schaefer-Prokop, a chest radiologist at Amsterdam University Hospital and Amersfoort Medical Centre, the Netherlands.
 Dr. Cornelia Schaefer-Prokop from Amsterdam. All images courtesy of the European Society of Radiology.
Dr. Cornelia Schaefer-Prokop from Amsterdam. All images courtesy of the European Society of Radiology.
Although the ideal environment of blamelessness and education might sometimes seem combative, anonymizing cases would help to reassure radiologists about the nonpunitive motives for holding such reviews. In the panel discussion one delegate volunteered that trust was built to such an extent in her department's review sessions that doctors would recognize case images and admit that they were the reporting radiologists.
Schaefer-Prokop pointed out that such reviews needed to be supplemented with communication among each other about ongoing cases, to -- as much as possible -- prevent mistakes before they occurred. This could take place through multidiscipline team meetings and more dialogue in daily work, ensuring that radiologists benefited from appropriate and accurate clinical information.
Despite best attempts to provide this accuracy, clinical information could point to something else and it is important to know the differentials, said Dr. Lorenzo Derchi, head of radiology at the University Hospital of Genoa, Italy.
He described how a 47-year old woman presenting with acute pain in the left flank and pelvis, unresponsive to pain relief, was sent to radiology with the suggestion of possible left renal colic. Ultrasound showed normal left and right kidneys, but a benign cyst in the right side of the uterus. A contrast-enhanced CT to rule out other nonlithiasic causes of renal colic showed the cyst, slight dilatation on the left, and a small amount of free fluid in the Douglas space, but radiologists still couldn't provide an explanation for the 'left renal colic.' As the patient was still in pain, surgery was performed, which found an ovarian serous cystoadenoma complicated by torsion.
 Dr. Lorenzo Derchi from Genoa, Italy.
Dr. Lorenzo Derchi from Genoa, Italy.
"Complications from torsion are associated with ovarian masses in 50% to 81% of cases. So why did we miss the diagnosis?" Derchi asked delegates. "First, because the symptoms 'suggested renal colic,' the renal and extrarenal ultrasound findings were normal, and because the cyst was considered incidental."
Other compounding factors were that the radiological considerations were not taken into account, or correlated to the clinical considerations; visible mass or enlarged edematous ovary and free pelvic fluid are associated with strong pelvic pain and predictive of torsion. Double reading was offered as another defense against errors; even a resident's fresh pair of eyes spotting something missed by a senior colleague, regardless of whether the interpretation was correct, was better than not seeing it at all.
"It's an odd paradox that screening mammograms in which 98% show normal findings are the only images subject to routine double reading in the U.K.," said Dr. Alan Freeman, an abdominal radiologist at Addenbrooke's Hospital in Cambridge, U.K.
Increasing image production meant that double reading as a practice solution was unrealistic in many instances such as chest x-ray. The sheer volume of slices made CT readings more prone to mistakes, accounting for 65% of all radiological reporting mistakes. Compounding this is a shortage of radiologists, resulting in hurried reading. Responding to this issue raised by session moderator Dr. Marc Zins, from Saint-Joseph Hospital in Paris, Schaefer-Prokop said that radiologists needed to adjust their reading processes, and use widely available three-dimensional tools. Freeman added that reading in a hurry was always a mistake. If adequate time could not be allocated, doctors should refuse to read images, as he learnt personally.
One particular case Freeman recounted to delegates was of an 88-year-old woman who presented with acute abdominal pain. The case came to him late in the afternoon when a trusted colleague wanted to discuss what he was certain was bowel ischemia in an otherwise healthy patient. At around 16:30 Freeman suggested a CT, in which he saw nothing to discount ischemia. Coronal and sagittal views seemed to show one major vessel supplying her gastrointestinal tract. As Freeman rushed to catch his five o'clock lift home, the patient was referred to the surgeons. On the next day, they performed a laparotomy and found adhesive disease, revealing in tandem a previous history of myomectomy and appendectomy.
 Dr. Alan Freeman from Cambridge, U.K.
Dr. Alan Freeman from Cambridge, U.K.
He considers his four major mistakes to be, first, reading images with preconceived ideas -- in this case suggested by his friend.
"A teleradiologist would not have been influenced like this," Freeman said, recommending delegates also attended Monday's session on teleradiology "For Better or for worse."
The second mistake was hurrying. The radiologist who acts in haste, repents at leisure, he warned. After this came mistaking radiology signs in axial and coronal views, and the fourth error was misinterpreting anatomy. Viewed retrospectively, the image depicted a variation of the hepatic artery coming off the supra-mesenteric artery.
Freeman also cited another mistake of offering a "no ifs or buts" diagnosis in reports: One such unquestionably described a CT colonography as demonstrating the presence of a T3 4-cm polypoid tumor arising from the anterior wall of the transverse colon. Repeated colonoscopies performed by the surgeon showed the disappearance of the "tumor." He concludes that it was probably chewing gum!
While perception and individual bias can impede objective reporting, technical reasons can hamper diagnosis in ultrasound, specifically of upper pole tumors, according to Derchi. Sagittal and axial views of the upper pole cannot provide a good means of evaluation, without coronal planes. Psychological "satisfaction of search" syndrome may also jeopardize diagnosis.
"When reading or performing an examination, once you discover a finding that explains symptoms, your attention drops and you may miss associated findings. In seven patients with two renal tumors each, one large and one small, the small one was only seen in one patient," he said.
Size, echogenicity, position of tumors, and incomplete scanning techniques that don't include the three scan planes can yield false negative ultrasound exams, he explained.
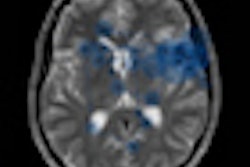
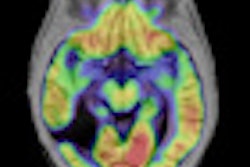
Detection errors were most often a question of perception and can be minimalized by comparison with previous studies, structural analysis of critical areas -- in the chest these being the upper lobes, the perihilar region, and the back, according to Schaefer-Prokop. Grayscale reversal and digital processing tools also help optimize data.
In terms of interpretation errors, causes were often insufficient knowledge of clinical history, absence of previous studies, the presence of a more obvious abnormality, and a lack of experience in the reader. "Not everything that looks like a tumor is a tumor," she said. "You don't want to get sued by the man who thinks he's dying of bronchogenic carcinoma and spends all his money, only to find that the lesion disappears because you missed the infectious disease that caused it."
Originally published in ECR Today March 6, 2011.
Copyright © 2011 European Society of Radiology