Perfusion imaging is proving increasingly useful for analyzing the biological behavior of central nervous system diseases, particularly the hemodynamic features. Qualitative and quantitative information can now be acquired for evaluating pathoanatomical structures, and pathophysiological changes of the lesions.
Due to rapid technical developments, CT and MR perfusion is available on most modern scanners. Furthermore, early and accurate diagnosis is a requisite condition for the successful treatment of vascular diseases, and perfusion imaging should not be limited to large centers, but should be used by any institution treating acute and chronic vascular diseases, according to Dr. Josef Vymazal, from the department of radiology at Na Homolce Hospital in Prague.
Ultrafast CT scanners can cover most of the brain with perfusion imaging, but there is widespread concern about radiation dose levels. In general, he thinks this concern is justified.
"CT is a significant source of radiation for the population of developed countries. However, newer CT scanners are able to deliver high quality images, while exposing the patient to less radiation," said Vymazal, who was scheduled to speak at Sunday's Special Focus Session on brain perfusion. "The radiation dose is also dependent on the type of examination performed. For example, newer scanners can perform examinations of the heart while exposing the patient to 10 times less radiation than older scanners."
MRI has the advantage of performing a contrast agent-free perfusion study using arterial spin labeling (ASL). ASL describes a group of MR techniques that allow noninvasive perfusion imaging, i.e. without the application of an exogenous contrast agent. Blood water is labeled (by saturation or inversion) as it passes through a magnetic field gradient. As the labeled spins flow into the imaging slice, the tissue magnetization is altered and perfusion-weighted images may be generated, he explained.
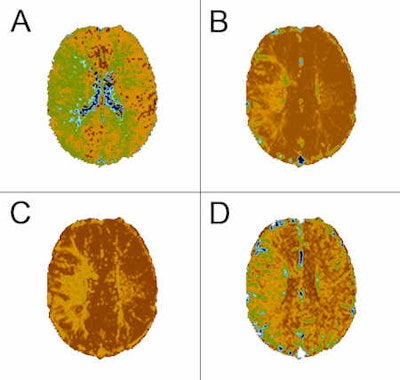
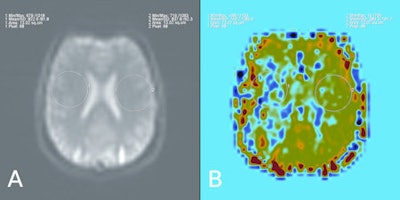 These six images show a comparison between contrast-enhanced perfusion and non-contrast perfusion using arterial spin labeling technique in a 34-year-old male with a chronic obliteration of the right middle cerebral artery. In the set of four contrast-enhanced perfusion images, A = time-to-peak (TTP), B = relative cerebral blood volume (CBV), C = relative mean transit time (MTT), D = relative cerebral blood flow (CBF). The other two are pulsed arterial spin labeling (QUIPPS II sequence) images. A: Sample of source data, signal in the circular region placed in the left hemisphere is 102% of that in the right. B: Relative cerebral blood flow, signal in the circular region placed in the left hemisphere is 271% of that in the right. Image courtesy of Dr. Josef Vymazal.
These six images show a comparison between contrast-enhanced perfusion and non-contrast perfusion using arterial spin labeling technique in a 34-year-old male with a chronic obliteration of the right middle cerebral artery. In the set of four contrast-enhanced perfusion images, A = time-to-peak (TTP), B = relative cerebral blood volume (CBV), C = relative mean transit time (MTT), D = relative cerebral blood flow (CBF). The other two are pulsed arterial spin labeling (QUIPPS II sequence) images. A: Sample of source data, signal in the circular region placed in the left hemisphere is 102% of that in the right. B: Relative cerebral blood flow, signal in the circular region placed in the left hemisphere is 271% of that in the right. Image courtesy of Dr. Josef Vymazal.ASL has found application in many research and clinical areas. One area that has received much attention is in the evaluation of patients with cerebrovascular disease, both in the initial assessment of perfusion as well as in evaluating treatment response. Vymazal believes the greatest limitation of these techniques may be that MRI is often not the preferred investigative method in acute situations. In non-emergency settings, however, ASL has the benefit of not only being a powerful, noninvasive perfusion imaging method, but also that it allows the investigative physician access to the many other high quality soft-tissue imaging techniques that can be applied in the MRI setting.
"I expect that CT will continue to be an essential part of the workup of acute cases," he predicted. "Hardware, software, and contrast development will continue to evolve at a rapid pace. This will maintain the current trend of increasingly superior images at lower and lower radiation doses. MRI will continue to evolve rapidly as well, as noninvasive techniques are further refined, and additional complementary protocols are further developed and perfected."
The term "perfusion imaging" is extensively used, but is in fact a misnomer because perfusion and blood flow are not the only imaging biomarkers of microvascular structure and function in common use, commented Dr. Alan Jackson, from the Division of Imaging Science and Biomedical Engineering at the University of Manchester, U.K. Indeed, in oncological applications, measurements of proportional blood volume, endothelial capillary permeability, or vessel size can be of equal or greater importance.
At Sunday's session, he was slated to review the biological rationale for using perfusion imaging in brain tumors, the methods available for the imaging of microvascular structure and function in brain tumors, and the methods for dynamic contrast-enhanced imaging and its analysis. He also intended to discuss the clinical applications, focusing on distinguishing abscess from tumor, differentiating tumor types, distinguishing glioblastoma from solitary metastases, and predicting grade, histological subtype, and prognosis in glioblastoma. He was also supposed to look at monitoring radiotherapy and predicting radiotherapy response, as well as applications in clinical trials of novel therapeutic agents, particularly antiangiogenic agents.
Originally published in ECR Today March 7, 2011.
Copyright © 2011 European Society of Radiology