Following a strong reaction from imaging specialists, the authors of new European guidelines on nephrogenic systemic fibrosis (NSF) have promised to consider revising their recommendations in a bid to restore the peace and avoid a protracted battle between radiologists and dermatologists.
The document about the diagnosis and treatment of sclerosing skin diseases from the European Forum of Dermatology (EDF) was published online on 9 August in the Journal of the European Academy of Dermatology and Venereology (JEADV). It has triggered a series of comments from leading MRI experts and has renewed discussion about the management of nephrogenic fibrosing dermopathy, a dermatologic form of NSF seen predominantly in patients with moderate-to-severe kidney failure.
The EDF guidelines state that no treatments with proven efficacy are available for NSF and recommend the following:
- The key preventive measure is avoidance of high-risk gadolinium-based contrast agents (GBCAs), especially in patients with an estimated glomerular filtration rate of < 30 mL/min.
- If an MRI scan with a GBCA is indispensable, a low-risk gadolinium medium should be the contrast agent of choice (table 3). The dose of the GBCA should be reduced to the minimum effective dosage for imaging.
- Based on the dialyzability of GBCAs, at least one full four-hour dialysis session should be performed after GBCA-based MRI in patients with renal insufficiency; this should remove 97% of the dose. Three full sessions of dialysis increase the GBCA clearance up to 99.7%
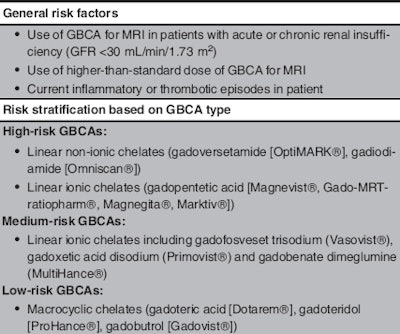 Risk stratification of GBCAs for NSF. GFR: glomerular filtration rate. Table courtesy of JEADV and Knobler et al.
Risk stratification of GBCAs for NSF. GFR: glomerular filtration rate. Table courtesy of JEADV and Knobler et al.Points of discord
Dr. Henrik Thomsen, professor of radiology at the Faculty of Medical and Health Sciences at the University Hospital of Copenhagen and chair of the Contrast Media Safety Committee (CMSC) board within the European Society of Urogential Radiology (ESUR), voiced his surprise at the document.
 Dr. Henrik Thomsen from Copenhagen.
Dr. Henrik Thomsen from Copenhagen."First of all, it is very late -- we needed it a decade ago when we had the last case of NSF in Western Europe and North America," he noted. "The guidelines produced by ESUR 10 years ago have been effective and should not be changed. In addition, the European Medicines Agency (EMA) changed its rules for chelates on 21 July so the EDF guidelines are out of date."
He said the risk stratification table needs to be updated because it listed GBCAs that were no longer produced and also because the EMA now advocates suspending the three high-risk GBCAs (gadodiamide/Omniscan, gadopentetic acid/Magnevist, gadoversetamide/Optimark) from the market, as well as restricting use of one medium-risk GBCA (gadobenic acid/MultiHance) to liver imaging. This leaves only three macrocyclic agents, considered to be low risk for NSF, available for general use.
Thomsen also rejects the EDF recommendation for hemodialysis for all patients with poor renal function.
"There is no evidence that dialysis for all patients with poor renal function protects them against NSF after contrast-enhanced MRI," he said. "For a patient on continuous ambulatory peritoneal dialysis it may cause a transfer to hemodialysis, while a one-off hemodialysis in a patient with poor renal function not yet on renal replacement therapy, may bring the patient earlier to dialysis."
 Dr. Georg Bongartz from Basel, Switzerland.
Dr. Georg Bongartz from Basel, Switzerland.
Furthermore, he said although GBCAs are well dialyzed, the statement that one four-hour dialysis session removes 97% of the injected material may not be accurate.
Dr. Georg Bongartz, vice chair of radiology and nuclear medicine at the University Hospital of Basel in Switzerland, echoed Thomsen's comments.
"If hemodialysis were to be performed in all these patients not yet undergoing it, morbidity and mortality would by far exceed the negative effects of gadolinium, especially of low-risk agents. The recommendation is based on a trial involving only 10 patients. This is not evidence-based medicine."
The response from dermatology
Lead author Dr. Robert Knobler, dermatologist and founder of the Photopheresis Center at the University Hospital of Vienna, noted the guidelines are an initial low-level document, compiled using informal methods.
He told AuntMinnieEurope.com the paper is aimed at raising awareness among dermatologists about sclerosing skin diseases and not at telling radiologists what to do. Moreover, because such guidelines take at least two years to prepare, there is always a risk that certain areas will not be up to date. He also noted the point about hemodialyzing all renal insufficiency patients after gadolinium-enhanced MRI was incorrectly worded and will be subject to an erratum note.
"The recommendation for hemodialysis was based on the literature, but the wording in our paper was unclear. Fortunately, we will be able to revise the guidelines within the next 24 months and clarify that hemodialysis after gadolinium-enhanced MRI should only be given to patients already undergoing regular hemodialysis," Knobler said. "We are open to discussion with our radiology colleagues and welcome their input."
To avoid future issues, there are plans to include a radiology expert for the next revision of the guidelines and to contact the ESUR's CMSC board and refer to its current guidelines, he added.
Multidisciplinary collaboration
The decision to include imaging specialists in the formulation of the revised guidelines already has been welcomed.
"For diseases such as NSF, which involve different specialties, guidelines should be developed with a multidisciplinary team. This would most likely have led to different conclusions and recommendations than are now formulated in the EDF S1-guidelines," stated Dr. Ilona Dekkers, clinical epidemiologist and radiologist-in-training at Leiden University Medical Center in the Netherlands, in an email.
Dekkers said a rebuttal letter to the JEADV would be of great value to the field, and also has offered to provide methodological input on guideline development.
Dr. Aart Van der Molen, an abdominal and musculoskeletal radiologist at the same facility, suggested that a withdrawal and revision of the current manuscript -- with modification to what he describes as its "far-fetched" NSF recommendations -- may save the authors a fierce discussion via letters to the editor in JEADV.
"The authors should consider the formulation of an evidence-based medicine guideline paper with clear descriptions of the methodologies used for establishing the guidelines, preferably in a multidisciplinary fashion, and without the recommendation for dialysis," said Van der Molen, also a member of ESUR's CMSC.
He added that the Radiological Society of the Netherlands is currently preparing a multidisciplinary guideline, Safe Use of Contrast Media part 2, with guidance on GBCAs and NSF, but it is not due for completion until the end of 2018.