Could macrocyclic gadolinium-based contrast agents (GBCAs) become the standard MRI protocol for pediatric patients? German researchers think so, after finding no measurable increase in signal intensity in key brain regions after multiple administrations in a study published in the October issue of Radiology.
The lack of greater signal intensity in the brains of young patients who received two commercially available gadolinium contrast products, compared with those who didn't receive contrast, indicates there is no retention or accumulation of gadolinium, even after multiple GBCA-enhanced MRI scans, according to a team led by Dr. Daniel Tibussek from Heinrich-Heine University and University Düsseldorf (Radiology, October 2017, Vol. 285:1, pp.223-230).
"Our results provide some evidence that brain gadolinium deposition does not occur to a measurable extent even after repeated administration of the macrocyclic GBCAs gadoteridol and gadoterate meglumine," Tibussek and colleagues wrote. "If results of our research are replicated in larger studies, the use of macrocyclic GBCAs may become the standard of care for pediatric patients requiring contrast-enhanced MR imaging."
The GBCA controversy
The debate over potentially adverse effects of GBCA administration and subsequent retention of small traces of gadolinium in certain brain regions is almost 4 years old now. Kanda et al ignited the controversy in December 2013 when the researchers noticed increased signal intensity in the dentate nucleus and globus pallidus among patients who had more than one GBCA administration.
Since then, several papers have contributed to knowledge about the differences between linear and macrocyclic GBCAs and how they could affect both adult and pediatric patients. Linear GBCAs are generally believed to have a higher risk of gadolinium deposition, but there appear to be differences between macrocyclic agents as well.
A March 2017 study by Radbruch et al found no evidence of increased signal intensity in the dentate nucleus of pediatric patients who had received the macrocyclic ionic GBCA gadoterate meglumine (Dotarem, Guerbet), findings echoed in an August 2017 study by researchers from South Korea. A December 2016 study reached similar conclusions, evaluating signal intensity among adults who received more than 20 administrations of gadoterate meglumine and the macrocyclic GBCA gadobutrol (Gadavist, Bayer HealthCare).
"To date, no detrimental impact of these depositions has been identified," Tibussek and colleagues wrote in the current paper. "However, the theoretical potential of long-term neurotoxic effects is of particular concern in infants and children, where the developing brain may be more vulnerable to gadolinium deposition."
Patients vs. controls
In this retrospective, single-center study, the researchers enrolled 24 pediatric patients younger than 18 years old with confirmed brain tumors. The subjects underwent at least nine GBCA-enhanced MRI brain scans with the macrocyclic agents gadoteridol (ProHance, Bracco Diagnostics) and gadoterate meglumine.
Mean patient age at the time of the first MRI exam was 8.25 years (range, 2-14 years); mean age at the last MRI scan was 12.7 years (range, 5-18 years). The mean number of GBCA-enhanced MRI exams was 14.2, with a minimum of nine administrations and a maximum of 24.
The researchers excluded participants with renal dysfunction; a history of brain hemorrhage, stroke, or ischemia; or central nervous system inflammatory disease. They also excluded those who had received a linear GBCA or who had undergone brain radiation.
In addition, the study included control patients who underwent unenhanced MRI brain scans between 2011 and 2015. The control subjects were matched by age and gender with their study counterparts.
All MRI exams were performed on a 1.5-tesla scanner (Magnetom Avanto, Siemens Healthineers) with a standard head coil. The MR imaging protocol included an axial T2-weighted sequence and a high-resolution T1-weighted 3D magnetization-prepared rapid gradient-echo (MP-RAGE) sequence.
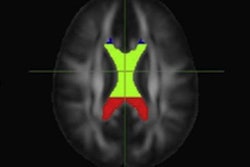
Because some brain tissue was distorted by lesions, signal-intensity measurements were only possible in the dentate nucleus for 18 patients. Measurements were available for the substantia nigra in 23 patients, and they were available in all 24 patients for the pons, globus pallidus, and pulvinar.
Two researchers independently measured mean signal intensity for each region of interest (ROI) in the right and left hemispheres of the brain of each subject. Paired t-tests were then used to calculate dentate nucleus-to-pons and globus pallidus-to-thalamus signal-intensity ratios and compare those values between GBCA patients and control patients. Statistically significant differences were assumed for p < 0.05.
ROI comparisons
The researchers saw no evidence of increased signal intensity in the dentate nucleus, pons, globus pallidus, substantia nigra, and thalamus on T1-weighted MR images between patients who had GBCA contrast and those who didn't.
| Mean signal-intensity ratios: Gadolinium contrast vs. no contrast | |||
| Brain region | GBCA patients | Unenhanced patients | p-value |
| Dentate nucleus-to-pons | 1.0083 (± 0.0373) | 1.0183 (± 0.01917) | 0.37 |
| Globus pallidus-to-pulvinar | 1.1335 (± 0.04528) | 1.1141 (± 0.07058) | 0.29 |
There also was no correlation between the number of GBCA administrations or the total amount of GBCA administered and signal change for any ROI.
"Our results provide some early evidence that repeated administration of the macrocyclic GBCAs gadoteridol and gadoterate meglumine does not result in measurable changes in nonenhanced T1 signal intensity as an indicator of gadolinium deposition in brain tissue," Tibussek and colleagues wrote.
They cautioned, however, that the results are limited by the small sample size and must be replicated in larger pediatric studies.
"Larger studies stratifying for age, underlying diseases, medications, and other confounders will therefore be necessary," they added.