Teleradiology workflow protocols appear to translate into healthcare delays, according to research conducted by a team from West Virginia University (WVU) in Morgantown.
The delays are not only frustrating for patients, but they also cost hospitals money, study lead author Bernardo Quiroga, PhD, a professor of supply chain management at WVU's College of Business and Economics, said in a statement released by the university. Quiroga's and colleagues' findings were published on 4 May in the Journal of Operations Management.
"Hospitals accrue direct costs by not having results available as soon as possible," Quiroga said. "However, the significant patient dissatisfaction that also arises from that delay is especially pertinent under Medicare's Value-Based Purchasing Program, which makes patient satisfaction scores critical to hospitals' revenues" (J Oper Man, May 4, 2023).
Hospital-based radiologists are salaried, but when they are working remotely, radiologists may earn money on what Quiroga described as a "piece-rate compensation scheme," for which they are paid for exam interpretations regardless of how long they take.
"Piece-rate compensation can be good for worker productivity and worker earnings -- but only if the scheme is set up correctly," he said.
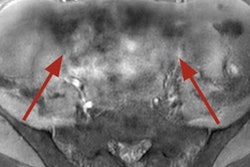
The investigators analyzed a teleradiology platform used across the U.S. that allows radiologists working from home to log in, view x-ray, CT, or MRI exams that need interpretation. Radiologists can then choose which of these exams to read and report on.
The research included more than 2.1 million imaging exams across 251 procedures conducted in 62 hospitals. Approximately 115 radiologists read the exams, which were categorized as "routine," "stat," "expedited," and "hyperacute." Most studies were classified as "stat" (that is, acute but not life-threatening).
The team found that the choices radiologists made about which exams to read were related to the studies' priority levels but also the perceived ratio of "pay-to-workload," or "how financially attractive the job is relative to the labor involved, or the job's 'bang for the buck,'" Quiroga said in a statement released on May 16 by WVU.
The findings "don't necessarily suggest that radiologists are putting medically urgent scans on the back burner," the university noted, but they may "tend to neglect studies with medium-level 'administrative' and 'operational' priorities." But in any case, "longer turnaround times created by this kind of poorly calibrated compensation scheme can delay results and patient admissions," WVU added.
How can the problem be resolved? Perhaps by changing the way studies are prioritized, Quiroga noted.
"A workflow platform could hide some routine procedures with high 'bang for the buck' when those studies are still far from their target turnaround times but expedited studies are about to hit their deadlines," he said. "That approach takes advantage of the platform's centralized nature and would be invisible to the radiologists. And, as long as the functionality is well-designed, that solution would be essentially costless."