
Breast and musculoskeletal (MSK) imaging accounted for over a third of legal allegations made against radiologists and trainees over the past decade, but the total number of cases remains low, according to Dutch figures published online on 17 February by European Radiology.
The Dutch Medical Disciplinary Court handled 48 allegations involving radiology practice between 2010 and 2019. A total of 46 allegations were made against radiologists, and two against trainees. The most common allegation (37.5%) was error in diagnosis, and most allegations were in breast and MSK (18.8% each), followed by interventional radiology, head and neck imaging, and abdominal imaging.
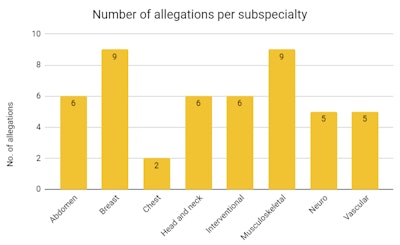 Allegations made against radiologists and residents and submitted to the Dutch Medical Disciplinary Court between 2010 and 2019.
Allegations made against radiologists and residents and submitted to the Dutch Medical Disciplinary Court between 2010 and 2019.In nearly 21% of verdicts, the allegation was judged to be partially founded, resulting in eight warnings and two reprimands. An appeal was submitted by the patient in 11 cases and by the radiologist in three cases. All appeals by patients were rejected, whereas two of the three appeals by radiologists were granted and previously imposed disciplinary measures were reversed.
Overall, the number of allegations was surprisingly low, Dr. Thomas Kwee, PhD, a radiologist at University Medical Center Groningen, told AuntMinnieEurope.com.
"It is hoped that this finding is reassuring to practicing radiologists, and will prevent or minimize the introduction of defensive medicine practices," he noted, adding that these allegations reflect patient dissatisfaction, but this doesn't often equal malpractice.
There is no real compensation culture in the Netherlands yet, but this does not mean that radiologists can disregard patient allegations or other expressions of dissatisfaction, added Kwee, who conducted the research with his twin brother, Dr. Robert Kwee, PhD, a radiologist at Zuyderland Medical Center, Heerlen/Sittard/Geleen.
"We should learn from all cases to maintain and improve the quality of healthcare," said Thomas Kwee. "In our opinion, the topic of malpractice is underexposed during radiology residency training in the Netherlands."
Failure is probably the No. 1 fear of most physicians, including radiologists, and as workload continues to increase each year, radiologists are at greater risk of making errors and being alleged for malpractice, he continued.
"Allegations may lead to defensive medicine -- an undesired phenomenon, because it is an important contributor to healthcare costs without adding any benefit to patients," he said.
The Kwee brothers do not have a medicolegal background and have neither served as an expert nor been involved in any cases, but they have worked together on several other projects.
"Society is changing, patients are becoming more demanding. Nowadays, patients can directly check their medical files online, including radiology reports," Thomas Kwee pointed out. "It will be interesting to investigate whether the number and types of allegations against radiologists change in the coming years."
Dutch legal context
The authors are not sure whether their results are applicable to other European countries, which have different legal systems. Also, they only included data from the Dutch Medical Disciplinary Court. Because patients may also proceed to the civil court, where they can file an allegation in parallel or separately from the Dutch Medical Disciplinary Court, the number of official allegations may be underestimated in the study.
There is no real financial obstacle or risk for a patient to file an allegation against a healthcare professional at the Dutch Medical Disciplinary Court, the authors explained.
"Patients can file an allegation for a total amount of 50 euros, which will be refunded if the allegation is judged to be (partially) founded. This very much contrasts with the civil court in the Netherlands, where the costs of the lawsuit process and the legal fees of the winning party have to be paid by the losing party if decided by the judge," they wrote.
Furthermore, the authors admitted they did not investigate the amount of time and attorney costs (83.3% of the 48 cases used an attorney during the court session) spent by defendants. In addition, they did not investigate the psychological impact of disciplinary measures on radiologists and whether these disciplinary measures achieved their main goal of maintaining and improving the quality of healthcare.



















