CHICAGO - Patients should be actively encouraged to know the names of their radiologists, and patient-driven care must become a vital part of radiologists' culture, however strange it may seem to them, RSNA 2013 delegates heard during the presidential address at Sunday's opening session.
RSNA President Dr. Sarah Donaldson's impassioned plea for closer partnerships with patients had added resonance because of her own background as a nurse, research assistant, and high-school cheerleader. She voiced her concern that as new technology has expanded, the medical profession has become less unified and is gradually drifting further and further apart, as shown by the separation of radiology and radiation oncology.
 RSNA President Dr. Sarah Donaldson.
RSNA President Dr. Sarah Donaldson.
"I know about the power of partnerships because I've witnessed them," noted Donaldson, a professor at Stanford University School of Medicine in Stanford, CA. "I look after children with cancer, and I can't imagine a more privileged thing to do."
Establishing a long-term relationship with patients makes work so much more rewarding, she added. She showed personal photos of her own patients, including Teddy, who was diagnosed with Hodgkin's lymphoma at the age of 10, but 24 years later has celebrated his sister's wedding and then his own. Spending 12 months learning about pediatric oncology at the Institut Gustave Roussy, a leading European cancer research center near Paris, in 1973 made her realize the importance of such relationships, she said.
Radiologists must accept responsibility for patient care beyond the rapid communication of imaging results, and they must remember that the most important partners are the patients themselves; when radiologists focus on patient care and become their partner, patients will come to understand radiologists' contribution to diagnosis and treatment and will become their advocate, she continued.
"The physician-patient bond that is well-developed in oncology can serve as a model for all of radiology, and confirms the gratifications that come from being a patient-oriented radiologist," Donaldson said. "Team-based practice promotes collaborative clinical and research programs, augments one's expertise, and builds careers. Professional interdependence promotes innovation and adds value to our collective endeavors."
But to meet today's demands for collaborative care and teamwork, she called for changes in radiology training and education and new ways to become more visible. "We can't afford not to do this," she said. "To be seen as equal partners, we must be at the table."
 Dr. Damian Dupuy.
Dr. Damian Dupuy.
The session began with a rendition of "You Raise Me Up" by the tenor Dennis McNeil. Arguably, this seemed somewhat out of place and random until the annual oration in diagnostic radiology was given by Dr. Damian Dupuy, director of tumor ablation at Rhode Island Hospital in Providence, RI. Standing on the shoulders of giants, a phrase coined by Isaac Newton, was the main theme of his lecture.
"The giants of radiology have given us the tools with which to work, and now we must collaborate better to ensure their appropriate use," he said. "The time has come for a reunification of spirit as well as intellect. Our patients and the medical community will reap the benefits of a stronger collaboration."
On average, radiology groups in the U.S. are almost three times the size of radiation oncology practices. Therefore, the support and input of these groups are essential to reach a stronger axis of collaboration, given the shared common interests and the marked synergy between many of the cancer treatments each possesses in its armamentarium, he explained.
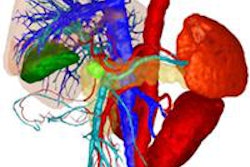
Advanced imaging of treatment response with contrast-enhanced imaging, perfusion and diffusion MRI, as well as PET/CT and PET/MRI is providing a clearer picture of tumor anatomy and pathophysiology, according to Dupuy. Radiologists can now place fiducial markers and brachytherapy catheters to provide more precise localization for stereotactic body radiotherapy techniques. Furthermore, imaging provides radiation oncologists with more accurate tumor targeting, reducing toxicity to adjacent normal and critical tissues.
"Combination therapies with external-beam radiotherapy or brachytherapy and thermal ablation technology have shown synergistic effects with promise for improved local control in larger tumors," he explained. "Intra-arterial radioembolics with yttrium-90 embolic agents utilize beta particles to destroy regional cancer of the liver."
Newer nonionizing techniques such as high-intensity focused ultrasound can provide stereotactic-like thermal destruction of soft-tissue tumors. Exciting preliminary results have shown potential in bone, breast, and prostate cancer, according to Dupuy.
"Radiation oncologists have great expertise at treatment planning with ionizing radiation. This experience has come from decades of research, as well as technical advances in computer science and photon delivery," he said, adding that radiologists who target tumors with ablative techniques have begun to realize the urgent need for 3D treatment planning.
Also included in the opening session was the following video, presented by Dr. Joy Sclamberg, president of the Chicago Radiological Society, a witty contribution from Chicago's radiologists to welcome RSNA 2013 attendees.
 |