There are a multitude of new challenges facing today's radiologist: increased pressure to improve patient safety, provide cutting-edge innovative technology, and collaborate more across clinical disciplines, while also lowering the cost of care. Often overlooked amongst these is the need to adapt to the increasing challenges of digitalizing healthcare.
Based on findings from a new study focused on the global health information exchange (HIE) market, this article takes a look at how large-scale IT infrastructure is already shaping and affecting radiology now and in the future.
Radiology has traditionally been ahead of the curve when it comes to use of IT. Early adoption of PACS and RIS over the last 15 years was at first painful, limited by doubtful administration and technical challenges. Yet across the majority of European hospitals and clinics, these systems have been installed and used, providing both clinical and financial benefit for healthcare providers. With second-, third-, and even fourth-generation iterations implemented, some radiologists may even have felt slightly smug as they watched other clinical disciplines struggle with first-generation installs and challenges.
Scale and interoperability: Painful inception of electronic health records
Today, things are far less simple. The principle of departmental IT solutions are quickly dying out, prompting a new era of enterprise interoperability and large-scale IT infrastructure. Healthcare provider focus on adopting electronic health records (EHRs) has often been the driver, with varied success. While it is clear that EHRs offer significant benefits in workflow and administration cost, their installation has often been costly and complicated. The sheer number of collaborators, security issues, and inability to interface with legacy systems has often led to painfully slow adoption, or abject failure in some high-profile cases.
Too often the core principle and wider long-term benefits of EHRs are missed or overlooked. EHRs being implemented today are not the final perfect solution for healthcare's IT woes. Instead, they are the initial steps toward a more important objective: true patient data interoperability.
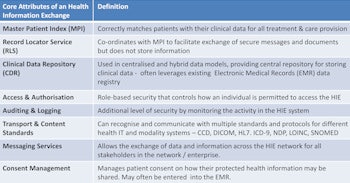
HIE is essentially the IT framework that will allow data interoperability across a far greater scale. Rather than just allowing image or patient record sharing across a hospital or even between hospitals, HIE will open the door to data sharing across regions, countries, and continents. Dare we say it -- it could even facilitate the use the overused "big data."
','dvPres', 'clsTopBtn', 'true' );" >

Click image to enlarge.
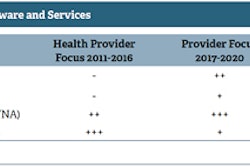
Development of HIE in EMEA.
Today, the HIE market is still in its infancy. Adoption across Europe has been limited and regionally disparate. In total, revenues attributed to HIE in 2013 were estimated at approximately $100 million U.S. (74 million euros), less than 11% of total PACS spend in Europe, the Middle East, and Africa (EMEA) and one-sixth of global HIE spending.
This mismatch in spending further highlights how far European healthcare providers have to go before we are even close to a "connected" European healthcare system. Regionally, Denmark and the wider Nordic countries are the stand-out HIE market performers, leading the adoption charge ahead of the U.K. For many countries, little to no spending has been made in adopting HIE.
So why should all this matter to radiologists -- surely this is up to IT administrators to manage and implement? Here are three reasons why HIE matters:
Improved collaboration between disciplines. Radiology has long been on the front line in trying to improve clinical diagnosis, yet all too often diagnosis is over-reliant on radiologist interpretation skills and the limits of current technology.
Access to best-of-breed departmental IT solutions. With the advent of broader enterprise IT and EHR implementation, many "best-of-breed" specialist departmental solutions are overlooked due to the current lack ability to interface with other IT systems. Yet HIE implementation could quickly change this. Due to the large scale and cost of investment needed to implement a regional or national HIE system, departmental IT system vendors (PACS, RIS, vendor neutral archive [VNA]) will quickly need to provide products that offer open interface with the incoming HIE. For the radiologist, this will mean more opportunity to again control the selection of departmental radiology IT and opt for best of breed.
Population health management (PHM) opportunity. Perhaps most importantly, HIE really does have the potential to form the foundation for improving health outcomes. Combining large-scale patient data will offer new opportunity for PHM tools, such as disease epidemiology analytics, predictive modelling, care management, and wider patient engagement. Small-scale trials across hospital networks (such as "The Esther Project" in Sweden) have already demonstrated the benefits and power of PHM tools in improving healthcare across a wider population. However, PHM provision relies heavily on HIE acting as the central exchange across health institutions and communities, interfacing and integrating a multitude of preinstalled IT systems.
Effective HIE implementation can allow far easier access to cross discipline information, pulling patient data and history from EHRs as well as all manner of multidisciplinary information together. Combining this information is itself powerful, offering a full view of conditions and patient history and past treatment. However, this should also prompt wider collaboration across disciplines, much in the same diagnosis and treatment planning for oncology has successfully adopted the multidisciplinary "tumor board" model. In doing so, it may also reduce the diagnostic burden on radiologists as well.
','dvPres', 'clsTopBtn', 'true' );" >
Click image to enlarge.
Core attributes of a health information exchange.
So while barriers continue to exist across Europe for Healthcare IT adoption, there are tangible benefits for radiologists and patients alike on the horizon. Admittedly, these changes will not happen overnight, with many of the challenges faced by radiologists adopting the first-generation PACS and RIS rearing again at a much greater scale. Yet radiology has a unique opportunity -- it has been there before and succeeded in adopting IT, despite the challenges. Therefore, radiology should be taking a leading role in encouraging HIE adoption across the hospital network, and with it, can also reap the long term rewards: improved collaboration, smarter PACS/RIS, and healthier patients.
Stephen Holloway is the associate director of medical devices and healthcare IT research at IHS.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.