A group from Russia has issued details about a series of simple, practical measures that can enable the medical imaging community to operate effectively in the COVID-19 pandemic.
Prof. Sergey Morozov, chief regional radiology officer of Moscow, and his colleagues at the Moscow Center for Diagnostics and Telemedicine (CDT), believe that the provision of radiology services in a pandemic should be based on these nine core areas:
- Infrastructure preparation (digital equipment and uniform resource identifiers operation)
- Quality training of radiologists and x-ray technicians
- Development of methodological materials and diagnostic protocols based on international experience
- Fast learning through distance education
- Integration of new protocols into the radiological information system in the form of study-report templates
- Regular discussion of complicated cases at online meetings and conferences
- Using a special dashboard to monitor performance
- Using a remote study reporting system
- Implementing artificial intelligence (AI) algorithms to help doctors.
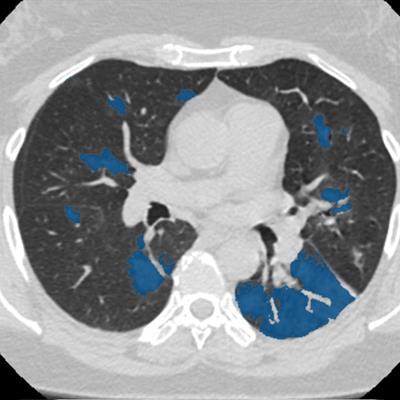
"In Moscow, 48 outpatient CT centers operate around the clock," Morozov noted. "From 13 April to 20 June, more than 170,000 chest CT scans were performed, and more than 82,000 cases of pneumonia with COVID-19 features were detected."
 From 13 April to 20 June, staff conducted over 170,000 chest CT scans at Moscow's 48 outpatient CT centers. All images courtesy of Prof. Sergey Morozov and Ilya Egorov.
From 13 April to 20 June, staff conducted over 170,000 chest CT scans at Moscow's 48 outpatient CT centers. All images courtesy of Prof. Sergey Morozov and Ilya Egorov.All cases of COVID-19 pneumonia have the following distribution by the degree of detected findings: CT-1 (mild), more than 49,000 cases (60%); CT-2 (moderate), more than 24,000 (29%); CT-3 (severe), more than 8,000 (10%); CT-4 (critical), more than 750 (1%).
Radiology departments are divided into "green" and "red" zones. Radiologists who provide CT scan reports and do not have face-to-face contact with patients are located in the separate clean "green" zone, while CT rooms are in the "red" zone.
"To compensate for the shortage of personnel, save time, and increase the device turnover, medical volunteers joined the team," he explained. "They meet patients, provide them with individual masks, escort them to exam rooms, and position them on radiographic tables."
Radiographers stay in the control room, setting up and running the exam, and a healthcare worker disinfects the equipment after completion of each exam. Staff working in the "red" zone are provided with class-three personal protective equipment (PPE). At shift changes, staff who are starting their duties do not overlap with staff who have completed them.
Support for radiographers
The CDT also provides psychological support to deal with the increased anxiety of staff. All radiographers have an opportunity to contact the center's psychologist to share his or her concerns, and more than 160 conferences have been held on this subject on the Zoom platform.
More than 1,000 diagnostic devices are connected to the unified radiological information service (URIS). At the beginning of the pandemic, only the equipment of Moscow state facilities was connected to the URIS, but the scanners of federal and private centers have now been added to the system.
According to Morozov, "Patients with a suspected coronavirus infection who come by appointment or are delivered by the ambulance to the outpatient CT center have a chest CT scan by physician's referral. Within 20 minutes, a radiologist, who may be in a different building, provides a study report, and the physician receives the information necessary for making a decision about the diagnosis and treatment tactics."
As of 20 June, the CDT had conducted over 300 online consultations on COVID-19, and more than 2,000 primary reports and 23,800 secondary reports were located in the URIS.
Effective use of AI
The use of AI has been essential, Morozov added.
"The study from the scanner is transferred to URIS right away and processed by algorithms. Then a radiologist receives both the original image and the image processed by AI. The doctor opens a worklist of studies on his/her computer which need to be interpreted. Preliminary study markings of suspected pathology made by AI services are available to a specialist," he said.
"When a radiologist opens CT scan images, he/she sees a copy of the original image, on which AI has highlighted pathological findings in red. This is how the algorithm draws the doctor's attention to the lung areas with a probable lesion," he continued. "To help with interpretation, AI can generate a report where it indicates the probability of viral pneumonia."
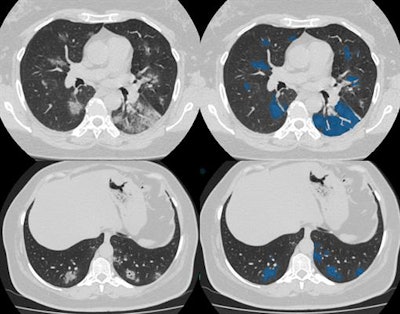 The AI solution is capable of learning from the database containing the CT scans with marked-up annotated lung lesions, aggregated by the Moscow Center for Diagnostics and Telemedicine.
The AI solution is capable of learning from the database containing the CT scans with marked-up annotated lung lesions, aggregated by the Moscow Center for Diagnostics and Telemedicine.The final conclusion, diagnosis, and further treatment, remain the sole responsibility of the doctor, he concluded.