Researchers from a top London facility have highlighted a simple and accurate COVID-19 diagnostic and prognostic imaging biomarker obtained from CT angiography (CTA) lung apices: the presence or absence of ground-glass opacification (GGO). They think their findings have major implications for management of patients with suspected stroke through early identification of COVID-19 and the limitation of disease transmission.
Diagnosis of COVID-19 relies on clinical features and reverse transcription polymerase chain reaction (RT-PCR) testing, but the sensitivity is limited, explained Dr. Juveria Siddiqui, consultant neuroradiologist at Kings College Hospital NHS Foundation Trust, and colleagues in an article posted online on 17 September by the American Journal of Neuroradiology. They evaluated carotid CTA as a potential COVID-19 diagnostic imaging biomarker.
 COVID-19 won't destroy our spirit: the interventional neuroradiology team at King's College Hospital, including nurses and radiographers. All images courtesy of Dr. Tom Booth, PhD.
COVID-19 won't destroy our spirit: the interventional neuroradiology team at King's College Hospital, including nurses and radiographers. All images courtesy of Dr. Tom Booth, PhD."At the very start of the pandemic, we noticed the ground-glass opacification (GGO) and thought this had the potential to be a useful biomarker," study lead and corresponding author Dr. Tom Booth, PhD, told AuntMinnieEurope.com. "However, what was very surprising was how this simple biomarker outperformed all the many other clinical markers we also analyzed."
"We also were surprised that the simplest measure -- i.e. the presence or absence of GGO -- was accurate and reliable compared to more nuanced and refined descriptions regarding, for example, exact location or whether focal or not," added Booth, who is a consultant neuroradiologist at King's College Hospital (KCH) and senior lecturer in neuroimaging in the School of Biomedical Engineering & Imaging Sciences at King's College London. "This is important as it is easy for radiologists who are not thoracic radiologists -- and likely clinicians and radiographers -- to interpret the sign."
Basics of the study
The group carried out a multicenter, retrospective study involving CTAs of 225 patients performed at three London hyperacute stroke units (KCH, Princess Royal University Hospital, and University College London Hospitals) between 25 March and 24 April 2020. The emergency stroke scan consisted of a CT of the head and neck blood vessels. The researchers evaluated the reliability and accuracy of candidate diagnostic imaging biomarkers. They analyzed the demographics, clinical features, and risk factors for COVID-19 and stroke using univariate and multivariate statistics.
Apical GGO was present in 22.2% (50/225) of patients. GGO had high interrater reliability (Fleiss k = 0.81; 95% confidence interval [CI], 0.68-0.95), and compared with RT-PCR tests, it had good diagnostic performance (sensitivity, 75% [95% CI, 56-87]; specificity, 81% [95% CI, 71-88]; odds ratio = 11.65 [95% CI, 4.14-32.78]; p = 0.001) on multivariate analysis.
| Diagnostic accuracy of imaging biomarkers on CTA in determining patients tested for SARS-CoV-2 (No. = 106) | ||||
| Sensitivity (95% CI) | Specificity (95% CI) | Positive predictive value (95% CI) | Negative predictive value (95% CI) | |
| Presence of GGO | 75% (56-87) | 81% (71-88) | 58% (41-74) | 90% (79-95) |
| Focal GGO | 46% (29-64) | 90% (81-95) | 62% (39-81) | 82% (72-89) |
| Bilateral GGO | 57% (37-75) | 82% (72-89) | 53% (35-71) | 84% (73-91) |
| Peripheral GGO | 68% (49-82) | 88% (79-94) | 68% (48-83) | 88% (79-94) |
| COVID-19-typical/indeterminatea | 64% (46-79) | 92% (84-94) | 77% (50-92) | 88% (74-95) |
In contrast, all other contemporaneous demographic, clinical, and imaging features available at CTA were not diagnostic for COVID-19, the authors wrote. The presence of apical GGO was an independent predictor of increased 30-day mortality (18% versus 5.7%, p = 0.017; hazard ratio = 3.51; 95% CI, 1.42-8.66; p = 0.006).
What's the significance?
The results show that when the researchers saw these changes in the top of the lungs during the emergency scan, they were able to reliably and accurately diagnose COVID-19, and the changes also predicted increased mortality, according to Booth.
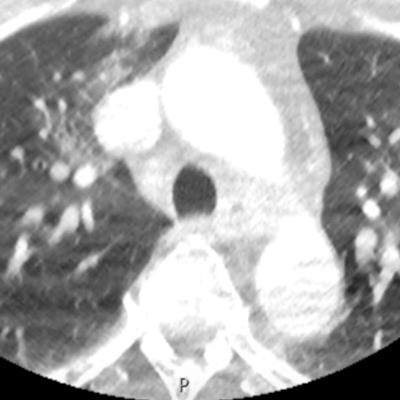
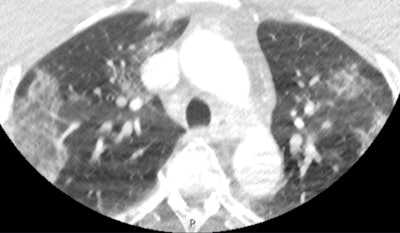 This scan shows apical ground-glass opacification in a patient with COVID-19. Despite the movement artifact that is not uncommon in acute stroke CT angiography, the biomarker is clearly present, alerting the treating team immediately that the patient has a high probability of COVID-19.
This scan shows apical ground-glass opacification in a patient with COVID-19. Despite the movement artifact that is not uncommon in acute stroke CT angiography, the biomarker is clearly present, alerting the treating team immediately that the patient has a high probability of COVID-19."This is particularly relevant given the limitations of currently available severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) reverse transcriptase polymerase chain reaction testing, as it takes time to complete the test and sometimes it is inaccurate," he noted.
The findings can allow earlier selection of the appropriate level of personal protective equipment (PPE) and attendant staff numbers, triage to appropriate inpatient ward settings, self-isolation and contact tracing, Booth continued.
"Additionally, our data have prognostic information given the increased mortality in those with lung changes shown in our cohort," he said. "These are useful results because the changes are simple for radiologists and other doctors to see. This is 'free information' from a scan intended for another purpose yet extremely valuable."
 Dr. Tom Booth, PhD.
Dr. Tom Booth, PhD.Overall, Booth remains convinced about how essential neuro-oncology diagnostics are when presenting patient information at multidisciplinary team meetings. On the neurovascular side, stroke imaging and aneurysm procedural work have become areas of considerable research interest. He has also investigated incidental findings -- both in terms of ethical/legal aspects and detection applied to neuroimaging.
As with all COVID-19 radiological research, the data are retrospective, whereas prospective data would be more robust, Booth pointed out. When all the legal and ethical approvals are in place, the next step is to run a prospective study, should a second COVID-19 wave come, he concluded.



















