The European Society of Radiology (ESR) has issued a detailed set of recommendations designed to promote the understanding and use of validated imaging biomarkers as decision-making tools in clinical trials and routine practice.
The 16-page document produced by the European Imaging Biomarkers Alliance (EIBALL), and endorsed by the ESR's Executive Council, was published on 29 August in Insights into Imaging. EIBALL is a subcommittee of the ESR's Research Committee, and its mission is to facilitate imaging biomarker development and standardization as well as promote their use in clinical trials and in clinical practice by collaboration with specialist societies, international standards agencies, and trials organizations.
"Both radiologists and clinicians are wary about using biomarkers," lead author Prof. Nandita deSouza told AuntMinnieEurope.com. "They are often acquired with very different imaging protocols, which make the quantitation across sites and equipment variable. Understanding this variability and the evidence for appropriate biomarker use would greatly help those who wish to incorporate these quantitative techniques into research or clinical use to make decisions when faced with individual patients."
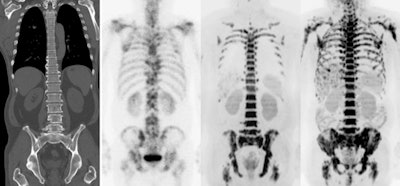 Multi-modality imaging of the skeleton shows secondary deposits in bone. Diffusion-weighted MRI (far right image) is a quantitative technique from which a biomarker called the apparent diffusion coefficient can be derived either from specifically segmented regions or from the whole skeleton. Image courtesy of Prof. Nandita deSouza.
Multi-modality imaging of the skeleton shows secondary deposits in bone. Diffusion-weighted MRI (far right image) is a quantitative technique from which a biomarker called the apparent diffusion coefficient can be derived either from specifically segmented regions or from the whole skeleton. Image courtesy of Prof. Nandita deSouza.Quantitation is going to increase as artificial intelligence (AI) comes on line, and making sure it is robust and meaningful is going to be hugely important, added deSouza, who is a professor in translational imaging and co-director of the Cancer Research UK Clinical Magnetic Resonance Research Group at the Institute of Cancer Research.
EIBALL is developing a web-based biomarkers inventory that will be available to anyone on the ESR website. EIBALL works with and seeks endorsement by specialist societies such as the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), the European Society of Gynaecological Oncology (ESGO), and the European Society for Breast Imaging (EUSOBI) for creating this inventory.
Also, EIBALL is working closely with its North American counterpart, the Quantitative Imaging Biomarkers Alliance (QIBA). The two groups both work towards setting benchmarks for imaging biomarker quantitation. They meet regularly to contribute to each other's work and ensure their goals are aligned.
"The ESR strongly supports this process, and gives EIBALL a platform for presenting developments at ECR every year," she pointed out.
Need for harmonization
In an era of machine learning and AI, it is vital to extract quantitative biomarkers from medical images that inform on disease detection, characterization, monitoring, and assessment of response to treatment. Quantitation can provide objective decision-support tools in patient management, but the quantitative potential of imaging remains underexploited because of variability of the measurement, lack of harmonized systems for data acquisition and analysis, and crucially, a paucity of evidence on how such quantitation potentially affects clinical decision-making and patient outcome, according to the authors of the EIBALL report.
Having looked at the use of semiquantitative and quantitative biomarkers in clinical settings at various stages of the disease pathway -- including diagnosis, staging, and prognosis, as well as predicting and detecting treatment response -- they feel strongly that measurement variability needs to be understood and systems for data acquisition and analysis harmonized before using quantitative imaging measurements to drive clinical decisions.
Semiquantitative readouts of scores based on an observer-recognition process are useful here. For example, MRI scoring systems for grading hypoxic-ischemic injury in neonates using a combination of T1-weighted imaging, T2-weighted imaging, and diffusion-weighted imaging have shown that higher postnatal grades were associated with poorer neurodevelopmental outcome, the authors noted.
In cervical spondylosis, grading of high T2-weighted signal within the spinal cord has been related variably to disease severity and outcome. In common diseases such as osteoarthritis, where follow-up scans to assess progression are vital in treatment decision-making, such scoring approaches also are useful; web-based knowledge transfer tools using the developed scoring systems indicate good agreement between readers with both radiological and clinical background specialisms in interpreting the T2-weighted MRI data.
"MRI is more versatile than ultrasound and CT," they wrote. "It can be manipulated to derive a number of parameters based on multiple intrinsic properties of tissue (including T1- and T2-relaxation times, proton density, diffusion, and water-fat fraction) and how these are altered in the presence of other macromolecules (e.g., proteins giving rising to magnetization transfer and chemical exchange transfer effects) and externally administered contrast agents (gadolinium chelates)."
Perfusion metrics have been derived with arterial spin labeling, which does not require externally administered agents. The apparent diffusion coefficient is the most widely used metric in oncology for disease detection, prognosis, and response evaluation. Postprocessing methods to derive absolute quantitation are extensively debated, but the technique is robust with good reproducibility in multicenter, multivendor trials across tumor types, according to deSouza and colleagues.
Hybrid imaging
Quantitation of F-18 FDG PET/CT studies is mainly performed by standardized uptake values (SUVs), although other metrics such as metabolic active tumor volume and total lesion glycolysis are being introduced in research and the clinic.
"The most frequently used metric to assess the intensity of FDG accumulation in cancer lesions is, however, still the maximum SUV," they continued. "SUV represents the tumor tracer uptake normalized for injected activity per kilogram body weight. SUV and any of the other PET quantitative metrics are affected by technical (calibration of systems, synchronization of clocks, and accurate assessment of injected F-18 FDG activity), physical (procedure, methods, and settings used for image acquisition, image reconstruction, and quantitative image analysis) and physiological factors (FDG kinetics and patient biology/physiology)."
To mitigate these factors, guidelines have standardized imaging procedures and harmonized PET/CT system performance at a European level. Newer targeted PET agents are only assessed qualitatively on their distribution.
Future challenges
To become clinically useful, biomarkers must be rigorously evaluated for their technical performance, reproducibility, biological and clinical validity, and cost-effectiveness, the authors wrote.
Technical validation establishes whether a biomarker can be derived reliably in different institutions and on widely available platforms. Provisions must be made if specialist hardware or software is required, or if a key tracer or contrast agent is not licensed for clinical use, they stated. Reproducibility is very rarely demonstrated in practice because inclusion of a repeat baseline study is resource and time intensive. Multicenter technical validation using standardized protocols needs to be addressed after initial biological validation. Quantitative biomarkers can then be clinically validated, showing that the same relationships are observed in patients.
Increasingly, the role of imaging in the context of other nonimaging biomarkers needs to be considered as part of a multiparametric healthcare assessment. The integration of imaging biomarkers with tissue and liquid biomarkers is likely to replace many traditional and more simplistic approaches to decision-support systems.
"In an era of artificial intelligence, where radiologists are faced with an ever-increasing volume of digital data, it makes sense to increase our efforts at utilizing validated, quantified imaging biomarkers as key elements in supporting management decisions for patients," they concluded.
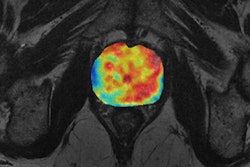
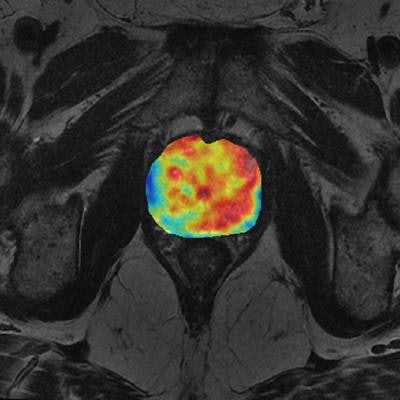
Editor's note: The image used to introduce this article on the home page illustrates multivariate analysis of prostate cancer from MR diffusion and perfusion acquisitions and generation of nosologic map by Euclidean-normalized algorithms. Image courtesy of Dr. Luis Martí-Bonmatí, PhD, and Dr. Angel Alberich.