Four-dimensional flow MRI can depict even subtle changes in left ventricular (LV) function, bringing new insight to the diagnosis of patients with mild left ventricular dysfunction and remodeling, concludes a study published on 17 August in PLOS One. Prior studies had detailed flow changes only in more severe disease, they said.
In their study, Swedish investigators acquired 4D flow and morphological data from 26 individuals with mild chronic ischemic heart disease and 10 healthy controls. Assessing both direct and nonejecting flow, and found that direct flow volume and kinetic energy (KE) proportions diminish with increased LV volumes, while nonejecting flow proportions increase.
"We have demonstrated that alterations in multidimensional intraventricular blood flow patterns and energetics may detect left-ventricular dysfunction even in subtle or subclinical left ventricular remodeling and dysfunction," wrote Dr. Carl-Johan Carlhäll in an email. Carlhäll is an associate professor of cardiology at Linköping University.
Mapping subtle dysfunction
The technique works across a spectrum of disease ranging from normal to mildly remodeled ventricles, the authors wrote. And 4D flow measures of volume and end diastolic kinetic energy showed a progressive shift in the proportions of both direct flow and nonejecting flow components, noted Carlhäll and colleagues Drs. Emil Svalbring, Alexandru Fredriksson, Jonatan Eriksson, et al from Linköping University in Linköping, Sweden.
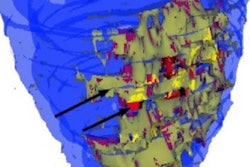
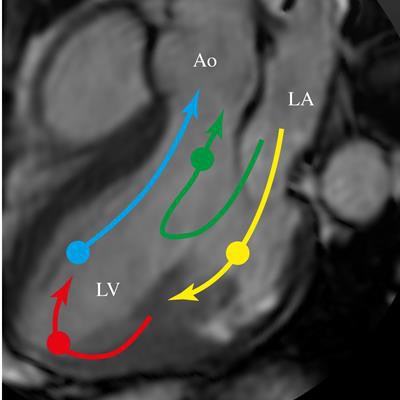
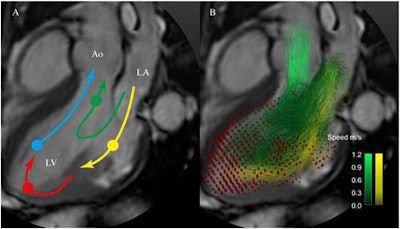 Schematic of the routes of the four LV flow components: direct flow (green), retained inflow (yellow), delayed ejection flow (blue), and residual volume (red). A semitransparent grayscale three-chamber image provides morphological orientation. Circles indicate the approximate location of the center of mass of each component at the time of end-diastole. Particle trace pathlines indicate routes of direct flow (green) and retained inflow (yellow). Red dots indicate the positions of the residual volume pathlines at end-diastole. Nonejected flow comprises the retained inflow and the residual volume. Ao, aorta; LA, left atrium; LV, left ventricle. Image republished with permission of PLOS One, 17 August 2016.
Schematic of the routes of the four LV flow components: direct flow (green), retained inflow (yellow), delayed ejection flow (blue), and residual volume (red). A semitransparent grayscale three-chamber image provides morphological orientation. Circles indicate the approximate location of the center of mass of each component at the time of end-diastole. Particle trace pathlines indicate routes of direct flow (green) and retained inflow (yellow). Red dots indicate the positions of the residual volume pathlines at end-diastole. Nonejected flow comprises the retained inflow and the residual volume. Ao, aorta; LA, left atrium; LV, left ventricle. Image republished with permission of PLOS One, 17 August 2016.A complex interplay of several features of normal and pathophysiological function combine to establish flow in the large vessels and cardiac chambers. Chamber configuration, material properties, load, and contractility all play a role in flow properties.
Previous studies have shown 4D flow MRI to be versatile for studying cardiovascular disorders where disruption of normal flow results from changes in flow components. The heart chambers' special challenges have spurred the development of special quantitative parameters for measuring intracardiac flow, the group wrote.
Proportions of functional flow components, kinetic energy, and flow structures have all been used to study left and right ventricular and atrial flow. Thanks to these efforts, 4D flow MRI has begun "expanding the assessment of ventricular function beyond conventional parameters including ejection fraction and diastolic filling patterns," Carlhäll and colleagues wrote.
Do trends in severe disease apply universally?
One prior 4D flow MRI study suggested that significant abnormalties in 4D flow volume and energy have occurred in patients with severely dilated and functionally depressed left ventricles. Another study confirmed this occurs in patients with moderate remodeling and depressed systolic function. But what about subtle disease?
"We hypothesized that these potentially adverse changes in flow volume and kinetic energy measured with 4D flow MRI would be detectable early in the course of disease, even in patients with only subtle LV dysfunction and enlargement," they wrote.
Spectrum of mild disease
The investigators acquired both 4D flow and morphological MRI data in 26 patients (16 men and 10 women) with moderate ischemic heart disease but no- to mild-systolic dysfunction and remodeling, as well as 10 healthy controls.
Twenty-four patients presenting symptoms for the ischemic patients included stable angina, fatigue, and dyspnea, while two of the patients were being followed for earlier myocardial infarction but had no current signs of ischemia.
A previously validated method was applied to separate direct flow through the LV to ejection from nonejecting flow, which remains in the chamber for at least one cycle. The investigators measured these components of end-diastolic volume.
4D flow and morphological MRI
The study team performed MRI to acquire 4D velocity data, morphological data, and late gadolinium enhancement images using a 3D Ingenia Scanner (Philips Healthcare).
The three-directional, 3D cine phase-contrast cardiac MR velocity data were acquired during a free-breathing gradient-echo pulse-sequence three-directional flow-encoding and retrospective cardiac gating.
The field-of-view was adjusted to cover the whole heart for the approximate 7 mm to 9 mm acquisition. Cine balanced steady-state free-precession (bSSFP) was used to obtain long- and short-axis images at 30 time frames during breathholds, following injection of Gadopentate contrast media.
- KE was calculated for the volume of each flow component and the entire whole left ventricular end-diastolic volume (LVEDV) over the cardiac cycle by using blood density and known velocities at different time points.
- LVEDV, left ventricular ejection fraction, left ventricular end-systolic volume, and left ventricular mass were calculated from segmented morphological cardiac MR images.
- 4D flow data were postprocessed and analyzed using in-house software.
Results showed that direct flow volume and KE both fell with increasing left ventricular end-diastolic volume index (LVEDVI) and LVESV-index (LVESVI). Direct flow volume was r = -0.64 and r = -0.74 (both p < 0.001). Direct flow KE was r = -0.48, p = 0.013, and r = -0.56 (p = 0.003) depending on LVEDV cutoff.
The results showed that direct flow volume and KE fell with increasing LVEDV-index (LVEDVI) and LVESV-index (LVESVI) (direct flow volume r = -0.64 and r = -0.74, both p < 0.001; direct flow KE r = -0.48, P = 0.013, and r = -0.56, P = 0.003) depending on LVEDV cutoff.
Meanwhile, the proportions of nonejecting flow volume and KE rose with increasing LVEDVI and LVESVI. The nonejecting flow volume was r = 0.67 and r = 0.76 (both p < 0.001) nonejecting flow KE was r = 0.53 (p = 0.005 and r = 0.52, p = 0.006, depending on LVEDV cutoff).
Direct flow falls, indirect rises
The direct flow volume correlated moderately to left ventricular ejection fraction LVEDVI (r = 0.68, P < 0.001) and was higher in a patients with left ventricular end-diastolic volume > 74 ml/m2 versus those with LVEDVI <74 ml/m2, and controls (both p < 0.05).
Direct flow volume and KE proportions fall with increased LV volumes, at the same time the nonejecting flow proportions increase, the team wrote. A drop in the direct flow volume and KE at end-diastole suggests that changes in these new 4D flow-specific markers may be able to detect left ventricular dysfunction even in patients with subtle or subclinical LV remodeling.
Moreover, the research "fills a gap in the spectrum of heart failure patients studied with 4D flow MRI to date," the authors noted.
When combined with prior studies, these results show a clearer picture that the most efficient component of LV volume, direct flow, falls as LV volumes increase. At the same time, the nonejecting components of left ventricular end-diastolic volume increase.
Toward better outcomes
"These altered flow characteristics may provide incremental pathophysiological insights relevant to both diagnosis and therapy of failing hearts, and empower the detection of ventricular dysfunction in clinically compensated patients," Carlhäll wrote in his email.
Future plans include additional improvements in both acquisition and analysis of 4D flow data, which will enable larger clinical studies including multicenter studies, he wrote.