As researchers gain experience with CT myocardial perfusion imaging (MPI) while new alternatives emerge, they're finding MPI remains harder to read than fractional flow reserve CT (FFR-CT). But CT MPI still has a lot going for it, including its potential to reduce catheterizations in patients with suspected coronary artery disease, according to a German expert.
To be sure, new techniques are nipping at the heels of CT MPI. Some alternatives are simpler; others are more sensitive, but take longer to perform. CT MPI is changing too, as clinicians demand faster answers, Dr. Thomas Henzler told delegates at the International Society for Computed Tomography (ISCT) 2016 Symposium.
"Before one technique is really established we have the next technique," Henzler said. "The whole motivation for myocardial perfusion imaging is the same as for FFR-CT. CT is excellent at detecting stenosis, but a poor predictor of myocardial ischemia. Therefore we require tests for which we can increase the specificity and predictive value of coronary CT angiography for ischemia."
Which MPI?
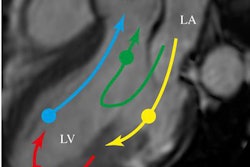
When people refer to MPI, they're actually talking about a variety of techniques -- but the principal dividing line in CT is between so-called static perfusion CT angiography and dynamic perfusion CT. Both can be performed with single-energy or dual-energy CT. Neither actually measures perfusion, but rather surrogates for it that examine iodine distribution at the point where the information is acquired, explained Henzler, who is chief of cardiothoracic imaging at the University Hospital Mannheim.
 Dr. Thomas Henzler from University Hospital Mannheim.
Dr. Thomas Henzler from University Hospital Mannheim.Static perfusion CT is hampered somewhat by the density of the myocardium itself, meaning that it's impossible to really discern how much density was contributed by the iodine. This limitation confers a small advantage on dual-energy CT because it enables the reader to selectively visualize the amount of contrast in the volume, he said.
Iodine distribution in the myocardium roughly corresponds to the arterial input function, and as a result, coronary CT angiography (CCTA) exams create a moment of peak enhancement in the myocardium, according to Henzler. This means a static or snapshot perfusion imaging technique may be sufficient, because it is at the time of peak enhancement that the small differences between normal and ischemic myocardium are maximized.
Between normal and ischemic myocardium "there's not much difference in information in the upslope [or] in the washout," he said. "The main difference is within those 12 to 20 seconds in which we acquire our CCTA data -- so this is the main argument for why some people think static perfusion might be enough for MPI."
A growing body of radiation exposure information also favors static perfusion imaging, which comes in at a radiation dose of about 5 mSv versus 10 mSv for dynamic perfusion CT. Whether it makes any sense to save 5 mSv of radiation exposure when trying to answer the critical question of coronary artery disease is another matter, he said.
One reason for the growing interest in FFR-CT may be the high quality of its studies. With MPI one sees relatively similar study results across exams: sensitivity and specificity ranging from the high 80th to 90th percentiles. Most studies have been conducted at single centers with cohorts of 30 to 100 patients -- and studies acquired with a variety of MPI techniques.
Similar to what researchers have found with perfusion CT, "when you do a meta-analysis there is no strong evidence that would favor one of the techniques," Henzler said. "I also think it's important that you have one value that gives you a yes or no answer -- and when we look at cutoff values for stress MPI for dynamic imaging there is a wide range, from 75 mL to over 105 mL, so there's no definite cutoff value that could be given to people. You can say, all right, use this cutoff value and it will give you ischemic myocardium."
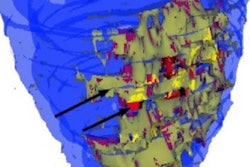
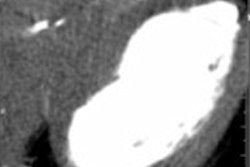
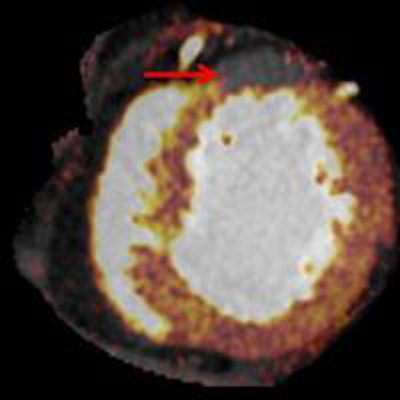
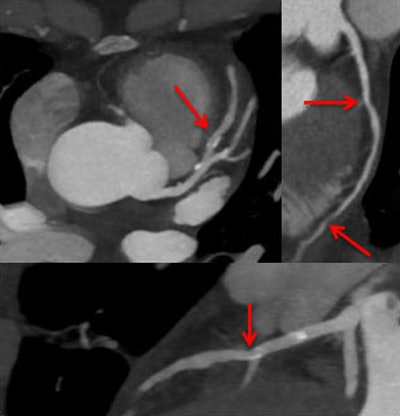 Cardiac dual-energy CT study in progress evaluates the potential of increasing coronary CT angiography's (CCTA) specificity by combining anatomic imaging and myocardial rest iodine distribution. Above, stenosis in intermediate left anterior descending (LAD) artery on morphologic CCTA images. Below, minor iodine distribution within distal LAD territory is a sign of hemodynamic significance of the lesion. Images courtesy of Dr. Thomas Henzler.
Cardiac dual-energy CT study in progress evaluates the potential of increasing coronary CT angiography's (CCTA) specificity by combining anatomic imaging and myocardial rest iodine distribution. Above, stenosis in intermediate left anterior descending (LAD) artery on morphologic CCTA images. Below, minor iodine distribution within distal LAD territory is a sign of hemodynamic significance of the lesion. Images courtesy of Dr. Thomas Henzler.When creating MI images, previous studies have shown it's better to calculate the myocardial blood-flow ratio manually rather than using absolute myocardial flow to calculate the effects of the stenosis. Calculating the myocardial blood-flow ratio better differentiates myocardium at risk, and could have other potential benefits.
Role in microvascular disease
"Maybe myocardial perfusion imaging might be of interest in microvascular disease," Henzler said. Vliegenthardt et al looked at different risk factors such as diabetes, hypertension, and hyperlipidemia and found differences in patient populations when risk factors were present compared with the control group, so the authors concluded in the setting of microvascular disease, CT MPI might be helpful in detecting myocardial differences among the patient groups.
Key arguments against stress and rest MPI include that it is a very long procedure that can't be performed in less than 40 minutes, Henzler said. His group, led by Meinel and colleagues, studied rest and stress and also delayed enhancement imaging to determine if everything was really necessary.
"Delayed enhancement didn't add any diagnostic information, and when you use rest you have high sensitivity but specificity below that of stress imaging," he said. Whether the additional specificity is needed is certainly worth discussing, "but interestingly we misclassified most perfusion deficits that were reversible using rest and stress -- and maybe this is because iodinated contrast also has some vasodilating effects that are responsible for the misclassification, and there are some risks in classifying [reversible] perfusion defects as fixed perfusion defects," Henzler said.
Maybe simple and quick is the best way to go. In a study published in February, Osawa and colleagues from Japan used only CCTA and myocardial iodine distribution images at rest, Henzler said. What they found is this simple technique was able to reclassify 38% of false-positive findings to true negatives -- by virtue of normal iodine distribution alone.
"This is the way we are currently going, doing [dual-energy CT] studies for coronary angiography and then looking for stenosis and taking iodine in the myocardium as additional information," he said. "We know this is not the perfect approach, but we also know there are viability tests and also tremendous progress in cardiac MRI that can give us information that is ... relatively fast and no longer than a standard CCTA. MPI has the potential to reduce the number of diagnostic catheterizations and you can assess true negative findings on CCTA."
There's a need for standardizing the technique analysis and providing cutoff values, and this technique may not require stress imaging, he concluded.