EuroMinnies finalists, page 2
Most Significant News Event in European Radiology
Dutch debate pros and cons of contrast-enhanced mammography and MRI for screening women with dense breast tissue
In early 2021, the heated discussion over the benefits and drawbacks of contrast-enhanced mammography and MRI for screening women with dense breast tissue was big news in the Netherlands, and it was the subject of a lively debate and vote in parliament.
The issue came to prominence when the Dutch Health Council (Gezondheidsraad) decided against implementing breast MRI screening. The group suggested that contrast-enhanced mammography should be explored as a potential alternative through a new trial.
Then a member of the Ministry of Health subcommittee appeared to undermine the official recommendations of the Health Secretary by proposing that women with dense breast tissue undergo MRI for screening and be told about their breast density, in addition to planning for the contrast-enhanced mammography trial recommended by the Health Council.
The Dutch Society of Radiology (NVvR) welcomed the development, but some radiologists expressed mixed feelings on the long-term role of both MRI and contrast-enhanced mammography in screening.
 Implementation of MRI screening will have some challenges, notes Dr. Marc Lobbes.
Implementation of MRI screening will have some challenges, notes Dr. Marc Lobbes."In practice, implementation of MRI screening will have some challenges," Dr. Marc Lobbes, PhD, a breast radiologist at the Zuyderland Medical Center and the Maastricht University Medical Center in the Netherlands, told AuntMinnieEurope.com.
The cost of screening will increase significantly as an estimated 80,000 additional MRI exams will need to be performed each year, and screening radiologists might have to increase their experience as the DENSE trial (November 2019, New England Journal of Medicine) involved the most experienced Dutch MR radiologists. More installations will be required and need to be serviced, and a shortage of qualified technicians exists. Also, when compared with contrast-enhanced mammography, acquiring and viewing the exams is time-consuming, according to Lobbes.
It will be intriguing to see if this issue resurfaces in 2022.
Ransomware attack on Irish health service causes disruption
Imagine having to run an imaging service without a PACS -- that's the chilling prospect that faced Irish radiologists in May 2021.
The Health Service Executive (HSE), the government agency responsible for the publicly funded healthcare system in Ireland, announced on 14 May that a "very sophisticated" ransomware attack had occurred and the HSE's IT systems had been shut as a "precautionary" measure.
"This has caused some disruption to our services. Most healthcare appointments will go ahead as planned, but x-ray appointments are severely affected," the HSE stated. "Following an initial assessment, we know this is a variant of the Conti virus that our security providers had not seen before. A ransom has been sought and won't be paid in line with state policy."
Dr. Adrian Brady, first vice president of the ESR and consultant radiologist at Mercy University Hospital in Cork, described the situation at his own facility.
 Dr. Adrian Brady.
Dr. Adrian Brady."We can keep the bare minimum emergency service going for a few days, but it's a struggle, and very limited and limiting," he told AuntMinnieEurope.com. "All IT systems are off-network, so we have no functioning RIS or PACS. We can do some imaging but can only view studies on modality-specific monitors -- e.g., view CTs on the screens in the CT scanning room. We can't disseminate studies, or issue formal reports."
The impact on radiology services has been "in a word, HUGE," reported Dr. Leo Lawler, consultant diagnostic and interventional radiologist and clinical director of radiology at the Mater Hospital in Dublin.
"All normal workflow ceased. We are limited to looking at imaging on the scanners. We are figuring out various workarounds to issue and communicate reports using various apps and in-house IT that is not connected to the internet," he said. "Virtually all our IT systems that had any connection to the internet were shut down including our national PACS and other systems as well as email. We have figured out business continuity, but it is slow, imprecise, and lacking correlation and comparison with other studies."
This disruption continued for several weeks, if not months, and it came just when radiologists were working round-the-clock to tackle the backlog of scans resulting from the COVID-19 pandemic. The incident has served as a warning and a wake-up call for the global imaging community about the devastating impact of cyberattacks on clinical practice.
Scientific Paper of the Year
Impact of specificity on cost-effectiveness of screening women at high risk of breast cancer with magnetic resonance imaging, mammography and ultrasound. Kaiser CG et al, European Journal of Radiology, 29 January 2021.
This German study showed that MR mammography (MRM) is a cost-effective alternative to mammography for yearly screening of high-risk cancer patients.
A team from the University Hospital of Mannheim found that screening with mammography versus MRM and treatment resulted in overall costs of $36,202 (31,948 euros) versus $39,051 (34,462 euros) and a cumulative effectiveness of 19.53 quality of life years (QALYs) versus 19.59 QALYs. This led to an incremental cost-effectiveness ratio (ICER) of $45,374 (40,042 euros) per QALY for MRM.
 Dr. Clemens Kaiser.
Dr. Clemens Kaiser."An interesting result from this study is that according to our analysis there are far less cost-effective imaging techniques than MR. A society that is willing to afford ultrasound as a screening tool should be far more willing to 'invest' in MRM," said lead author Dr. Clemens Kaiser, whose father, Prof. Dr. Werner Kaiser from Jena, Germany, was a pioneer in breast MRI.
The authors also found that ultrasound and the combination of mammography and ultrasound had ICER values higher than the willingness to pay threshold (WTP) of $100,000 (88,257 euros) per QALY.
In sensitivity analyses, MRM was still cost-effective in screening high-risk patients as long as the technique's specificity did not drop below 86.7%.
A probabilistic sensitivity analysis also showed higher costs on average, as well as higher effectiveness of the MRM strategy in high-risk patients. Another analysis showed that a willingness to pay threshold of more than $30,400 (26,830 euros) per QALY indicated that MRM was cost-effective in most iterations.
While a direct comparison of mammography and MRM showed the latter had higher costs, it also had a higher cumulative effectiveness in most cases.
Kaiser told AuntMinnieEurope.com last year that these results suggest that there is "seemingly no reason" not to use MRM as a screening tool for patients with dense breasts.
"Cost issues are one of the major concerns against using MRM in a broader set of indications, which is why we have been trying to fill the data gap. This paper indicates that MRM is diagnostically superior as well as cost-effective," he added.
It is important to mention that the data suggest that MRI should be performed by radiologists, who are at least able to maintain 86% specificity in order to keep up the monetary advantage reliably, Kaiser continued. This means that MR mammography should simply not be performed by just "anyone", but somebody with experience.
"Just like any other imaging technique, MR mammography can only be as good as the radiologist reader," he said. "In expert hands, however, MR mammography could really be able to revolutionize breast cancer prevention."
To read the whole article, go to the European Journal of Radiology website.
Magnetic resonance imaging incidents are severely underreported: A finding in a multicentre interview survey. Kihlberg J et al, European Radiology, 20 July 2021.
MRI-related incidents tend to be "greatly" underreported, which could lead to catastrophic outcomes, according to a Swedish study published in July in European Radiology.
A team led by MRI radiographer Johan Kihlberg, PhD, from the Center for Medical Image Science and Visualization (CMIV) in Linköping, said considering their results, major educational efforts are needed to enhance a culture of safety in MRI.
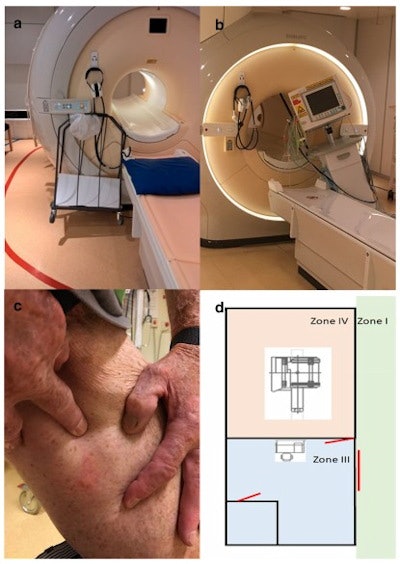 Examples of MRI accidents. (A) A trolley is stuck on the magnet. (B) A patient monitor is stuck on the magnet. (C) A patient experienced a blister in the groin. (D) Safety zone II is missing (the red lines represent the three doors to the unit). Images courtesy of Johan Kihlberg, PhD, and colleagues and European Radiology.
Examples of MRI accidents. (A) A trolley is stuck on the magnet. (B) A patient monitor is stuck on the magnet. (C) A patient experienced a blister in the groin. (D) Safety zone II is missing (the red lines represent the three doors to the unit). Images courtesy of Johan Kihlberg, PhD, and colleagues and European Radiology.Researchers interviewed managing radiographers from 13 sites included in the study. Questionnaires filled out by the radiographers showed that only 38% of incidents were reported formally, suggesting that about 100 incidents remained unreported. Among these incidents reported were radiofrequency burns, but attitudes about expecting to be burned while working in the field imply that responders felt they were unnecessary to report.
"One site routinely reported scanned patients that later were found to have coins or paper clips in their clothing," researchers said. "This reflects an accurate interpretation of Swedish law that defines incidents as 'Unwanted events that happened or could have happened.' "
About half of the responders were reportedly unaware of the EU directive 2013/35, which was adopted into the occupational health law in Sweden in 2016, researchers said.
However, the team also found that MRI knowledge increased because of the availability of MR physicists at the site, which decreased the risk for incidents. Almost all radiographers in the study also expressed concern about MR safety knowledge for their respective radiologists.
"MR-specialized radiographers have a very diverse background, and not surprisingly, MR knowledge varied substantially across the sites," the study authors wrote. "The entire process of maintaining MR safety requires collaboration between different professions such as radiographers, MR physicists, and radiologists."
To read the entire article, go to the European Radiology website.
Best New Radiology Device
Somatom X.ceed CT scanner, Siemens Healthineers
Unveiled in May 2021, the Somatom X.ceed CT scanner is adapted from the Somatom X.cite system that the company launched in 2019. The new system is optimized for emergency, cardiac, and interventional use, but it can also perform all-around imaging.
The Somatom X.ceed system bundles the same technologies into a more powerful CT platform, according to Jesus Fernandez Leon, global product manager for CT marketing at Siemens.
 Siemens highlights emergency applications among the capabilities of its new Somatom X.ceed CT scanner. Image courtesy of Siemens.
Siemens highlights emergency applications among the capabilities of its new Somatom X.ceed CT scanner. Image courtesy of Siemens.Both systems also include tablet computers that enable technologists to control the scanner's operation remotely, whether they are in the scanning room or the console room. Many technologists have found the tablet controls useful during the COVID-19 pandemic, Fernandez Leon added.
X.ceed supports dual-energy spectral imaging, as does the X.cite system, but Siemens has broadened the spectral field of view to 50 cm, compared with 42.5 cm on X.cite. This will give X.ceed users more flexibility in using spectral imaging, he said.
Somatom X.ceed is being marketed globally, but the company expects an initial emphasis on Europe and the U.S., with sales in China and Asia-Pacific to follow. On 19 January 2022, a spokesperson for Siemens said he could not disclose exact installation numbers, but confirmed the new CT scanner has already been installed in "many locations globally and is used there clinically, including locations in Europe."
Swoop 64mT MRI scanner, Hyperfine
The Hyperfine Swoop is a 64mT machine intended mostly for head injuries, but it also has applications in wrist, knee, and foot imaging. It can be located in smaller and more crowded spaces such as the intensive care and stroke units, outpatient centers, and pediatric departments.
The average scan for a patient is 35 minutes, and that includes T1, T2, fluid-attenuated inversion-recovery (FLAIR), and diffusion imaging with 3D slices and millimetric resolution, and the machine has to be integrated into the hospital's PACS.
As part of a research collaboration with the Bill & Melinda Gates Foundation, Hyperfine has installed Swoop systems at King's College London and Cardiff, U.K., plus other locations in Europe, according to the vendor's chief medical officer Dr. Khan Sidiqqui.
The company is currently in the process of applying for a CE Mark for the Swoop system, he added.
 Hyperfine is in the process of applying for a CE Mark for the Swoop system. Image courtesy of Hyperfine.
Hyperfine is in the process of applying for a CE Mark for the Swoop system. Image courtesy of Hyperfine."This solution is truly disruptive, in the sense that the technology allows for a paradigm change," said Mathieu Sarracanie, PhD, co-head of the Adaptable MRI technology center at the University of Basel, Switzerland, in a March 2021 article. "It has a small footprint and is also mobile. These machines don't need any specific siting and the cost is low. The con is that these devices are purpose-built, and some customers may see that as a disadvantage."
Pointing to Hyperfine's imaging capacity, he noted that gray- and white-matter contrast can show very high dispersion at lower field strength. This has been explored by researchers at the University of Aberdeen, U.K., who have generated some fascinating T1 contrast results in stroke patients thanks to a novel fast-field cycling MR scanner, he commented.
"Now is the time for ultralow-field MRI. The 0.55T machine could be a serious contender to the standard 1.5T as it is more compact and cost-efficient. Machines at even lower field strength will not replace MRI as we know it but will expand its use and bring it to other places that we don't know yet," Sarracanie added.
Best New Radiology Software
qp-Prostate AI software for prostate MRI, Quibim
Spanish image analysis software developer Quibim was founded by Ángel Alberich-Bayarri, PhD, and Dr. Luis Martí-Bonmatí, PhD. Its qp-Prostate product is an AI program to aid in prostate MRI reporting, from visualization to quantification. The software received 510(k) clearance from the U.S. Food and Drug Administration (FDA) in March 2021.
qp-Prostate is an image processing program designed for use by radiologists specialized in prostate imaging, urologists, and oncologists. Data and images are acquired through DICOM-compliant imaging devices and modalities. qp-Prostate doesn't perform diagnostic functions. Instead, it allows users to visualize and analyze DICOM data.
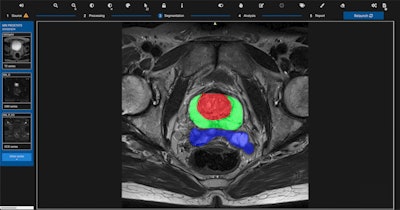 The qp-Prostate software at work. Image courtesy of Quibim.
The qp-Prostate software at work. Image courtesy of Quibim.The imaging processing software is PI-RADS v2.1 compliant and runs on off-the-shelf workstations. The software enables automated segmentation of the transitional zone, peripheral zone, and seminal vesicle regions of the prostate to aid in image interpretation and diagnoses, according to the company. Its application ultimately may reduce interpretation time and help define diagnosis per region.
Martí-Bonmatí, chairman of the radiology department and director of medical imaging at La Fe University and Polytechnic Hospital in Valencia, discussed the company's philosophy for developing AI in a session at ECR 2020. You can read that story here. qp-Prostate is currently being deployed at hospitals in the U.S. and Spain.
Medical Open Network for AI (MONAI), Nvidia and King's College London
Originally launched as a video graphics developer for computer gaming, Nvidia took its first steps in the medical imaging field in 2009 when it developed a 3D ultrasound visualization system for expecting parents to see their unborn child.
Today, the Santa Clara, California, company is working with King's College London in the U.K. on an open-source framework called Medical Open Network for AI, or MONAI, a toolkit for deep learning in healthcare imaging.
MONAI is designed to handle formats, resolutions, and metainformation of medical images, according to Nvidia. The first public release of the framework in 2020 provided domain-specific data transforms, neural network architectures, and evaluation methods for measuring the quality of medical imaging models.
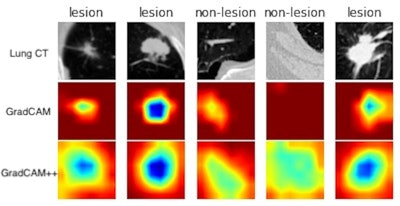
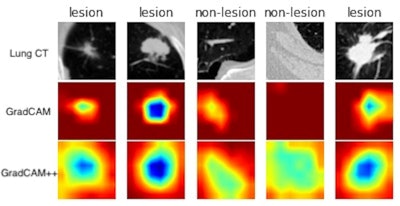 MONAI provides Class Activation Mapping (CAM), gradient-weighted CAM (Grad-CAM), and Grad-CAM++ application programming interfaces for both 2D and 3D models. The above example is generated by computing Grad-CAM and Grad-CAM++ from a lung CT lesion classification model. Image courtesy of Nvidia.
MONAI provides Class Activation Mapping (CAM), gradient-weighted CAM (Grad-CAM), and Grad-CAM++ application programming interfaces for both 2D and 3D models. The above example is generated by computing Grad-CAM and Grad-CAM++ from a lung CT lesion classification model. Image courtesy of Nvidia.The open-source code is based on the Ignite and PyTorch deep-learning frameworks and integrates libraries for tasks such as data processing, 2D classification, and 3D segmentation. Nvidia reports that MONAI can easily be added by researchers to their existing code; its customizable design enables modular components to be integrated into AI workflows.
Chief Technology Officer Jorge Cardoso of the King's College London AI Centre said in a recent blog post that such a comprehensive tool was missing prior to MONAI.
"Researchers need a flexible, powerful and composable framework that allows them to do innovative medical AI research, while providing the robustness, testing and documentation necessary for safe hospital deployment," he said.
The ultimate goal is to establish standardised practices for input and output processing and transformations, collaborative learning, evaluation, and benchmarking, as well as to define network architecture specific to healthcare imaging, according to the collaborators.
MONAI v0.6 became available in July 2021.
Best New Radiology Vendor
Lucida Medical, Cambridge, U.K.
A spin-off from the University of Cambridge in the U.K., Lucida Medical is developing artificial intelligence (AI) algorithms for cancer detection on MRI, focusing initially on prostate cancer.
Lucida's initial product -- Prostate Intelligence (Pi) -- makes use of radiogenomics, machine learning, and image-processing techniques to analyze and detect cancer on prostate MRI images. It generates a prostate cancer risk score, identifies candidate regions of interest for biopsy, and provides image segmentations.
In research presented at ECR 2021, the software was estimated to enable a 7% reduction in missed prostate cancers and a 24% decrease in unnecessary biopsies, according to the firm. Pi received the CE Mark in June.
In September, Lucida launched a retrospective validation study of Pi in collaboration with Hampshire Hospitals NHS Foundation Trust. The study will apply Pi to prostate MRI exams of up to 2,100 patients.
 (Left) Antony Rix, PhD, and (right) Prof. Evis Sala.
(Left) Antony Rix, PhD, and (right) Prof. Evis Sala.Lucida was co-founded in 2019 by AI expert CEO Antony Rix, PhD, and chief medical officer Prof. Evis Sala. Rix is an entrepreneur with 25 years' experience in software development whose first startup, Psytechnics, was based on his PhD in machine learning and was acquired by Netscout in 2011. Sala is a cancer imaging specialist from the University of Cambridge. Mark Hinton serves as the firm's chief technology officer, having been the former chief technology officer at Image Analysis Group.
The firm is also a member of the ReIMAGINE prostate cancer consortium and has raised millions of pounds in a seed capital investment from a group of investors led by XTX Ventures and Prostate Cancer Research. In June, Lucida joined GE Healthcare's Edison Accelerator program, which is aimed at supporting early-stage companies developing healthcare AI applications.
The company completed the integration of Pi with the NHS East Midlands Imaging Network (EMRAD), a group of 8 NHS Trusts in England, in partnership with GE Healthcare. This work took place through GE Healthcare's 2021 EMEA Edison Accelerator Programme, where Lucida Medical was one of six finalists selected from 350 applicants. The result was announced on 30 November 2021 at GIANT Health 2021 in London.
Radiobotics, Copenhagen, Denmark
With a focus on musculoskeletal radiology, Danish startup Radiobotics is creating a slew of artificial intelligence (AI) software applications to assess digital x-rays of bone and joints.
The company's first commercially available algorithm -- RBknee -- analyzes a standing postero-anterior knee radiograph to identify common radiographic findings associated with the diagnosis of osteoarthritis (OA): osteophytes, subchondral sclerosis, and joint space narrowing, according to the Copenhagen-based vendor. Its machine-learning algorithms then conclude whether OA is present.
 The four founders of Radiobiotics. From the left: Pavel Lisouski, Stine Mølgaard Sørensen, Mads Jarner, and Martin Axelsen.
The four founders of Radiobiotics. From the left: Pavel Lisouski, Stine Mølgaard Sørensen, Mads Jarner, and Martin Axelsen.RBknee is suitable for use in orthopedic or radiological settings. The software has received the CE Mark as well as U.S. Food and Drug Administration 510(k) clearance.
Radiobotics is also developing other musculoskeletal radiology AI software applications, including RBmarker and RBfracture. RBmarker is designed as a quality-control tool for x-ray laterality markers, while RBfracture evaluates x-rays for hip fractures.
The company's algorithms generate automated text reports and provide visual overlays on the images. In December, Radiobotics signed an agreement to make RBknee available on image exchange software provider TeleRay's platform.
Radiobotics has raised over $4 million (3.5 million euros) and was co-founded in 2017 by CEO Mads Jarner Brevadt, Chief Technology Officer Pavel Lisouski, Chief Strategy Officer Martin Axelsen, and Chief Operating Officer Stine Mølgaard. The company was also selected -- along with the other EuroMinnie Best New Vendor Finalist Lucida Medical -- for GE Healthcare's Edison Accelerator program, which is aimed at supporting early-stage companies developing healthcare AI applications.
Previous page | 1 | 2



















