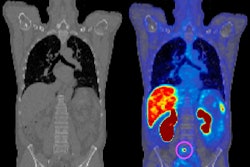
Prostate-specific membrane antigen (PSMA) PET imaging can improve the length and quality of life for patients with recurrent prostate cancer, according to a U.K. study published on 23 October in JAMA Network Open.
In a modeling study of simulated patients, compared with conventional imaging, PSMA-PET was estimated to lead to fewer deaths from prostate cancer, more life years, and more quality-adjusted life years (QALYs) per 1,000 patients.
“This decision analytic modeling study projected that upfront PSMA-PET for the imaging of BCR prostate cancer is expected to lead to more patient life years and QALYs and fewer deaths from prostate cancer,” noted lead author Natalia Kunst, PhD, of the University of York’s Centre for Health Economics.
Although studies have shown that PSMA-PET is highly effective for detecting prostate cancer, the long-term consequences of widely implementing the technique in patients with recurrent disease are unknown, the authors explained.
To address this gap in evidence, the researchers developed a decision analytic model to estimate clinical outcomes associated with PSMA-PET versus conventional imaging strategies, namely CT and bone scans.
The model simulated three alternative strategies that patients may encounter: immediate PSMA-PET without conventional imaging, PSMA-PET imaging as a reflex test if conventional imaging findings are negative or equivocal, and conventional imaging alone.
According to the analysis, per 1,000 patients PSMA-PET alone was estimated to detect 611 patients with metastatic disease, 140 patients with localized disease, and 249 patients with no radiographic disease.
Imaging with PSMA-PET as a reflex test if conventional imaging findings are negative or equivocal was estimated to detect 630 patients with metastatic disease, 144 patients with localized disease, and 226 patients with no radiographic disease per 1,000 patients.
Finally, conventional imaging alone was estimated to detect 297 patients with metastatic disease, 10 patients with localized disease, and 692 patients with no radiographic disease.
“Our results suggest that use of PSMA-PET alone or as a reflex test following negative findings with conventional imaging is expected to detect more than twice the number of patients with metastatic disease,” the group wrote.
The authors noted that to their knowledge, this study is the first to address outcomes of PSMA-PET in the setting of recurrence in the U.S. population and was informed by data from real-world settings.
To date, in the context of cancer imaging, relevant outcomes, such as overall survival or quality of life, are frequently not available due to a limited follow-up period, they added.
“Our findings highlight the need to consider longer evaluation horizons, as well as methodological strategies to inform preliminary boundaries at which imaging agents may yield improved patient outcomes,” the researchers concluded.
The full study is available here.