Researchers from Turkey have found that asymmetrical cortical enlargement on the side closer to the breast, abnormal microvascular pattern, and high cortex-hilum (C/H) ratio are independent predictors of axillary nodal involvement. Furthermore, close asymmetry is an eligible, easy-to-spot grayscale ultrasound finding to predict axillary lymph node (ALN) metastasis.
 Dr. Seda Aladag Kurt.
Dr. Seda Aladag Kurt.The study findings are easily applicable in breast clinics and will significantly benefit routine practice, first author Dr. Seda Aladag Kurt, a breast imaging specialist at Cerrahpașa Faculty of Medicine in Istanbul, told AuntMinnieEurope.com.
"Axillary staging is crucial for breast cancer staging," she said. "Consider paying attention to the side of asymmetrical cortical thickening in axillary imaging. If it is closer to the breast, it could be a warning sign for axillary metastases."
In an article published in European Journal of Radiology on 7 December, the researchers aimed to investigate the relationship between ultrasound findings and axillary node status, especially the side of thickening in the presence of cortical asymmetry.
Patients with biopsy-proven ALN metastasis were included in this study. A total of 281 patients with suspected metastatic ALNs who applied for diagnostic or screening purposes between January 2020 and February 2022 were evaluated. Inclusion criteria included the following: patients diagnosed with invasive breast carcinoma and patients who underwent sampling on suspicion of a metastatic ALN at initial ultrasound examination.
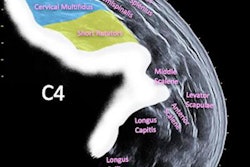
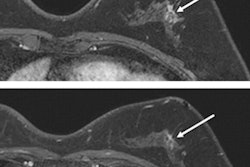
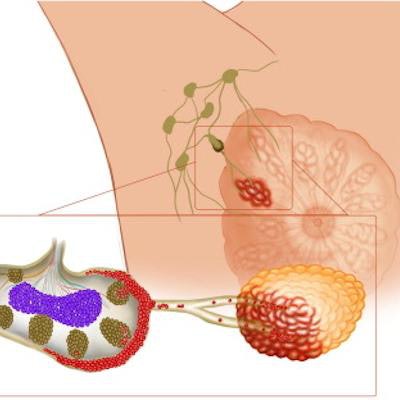
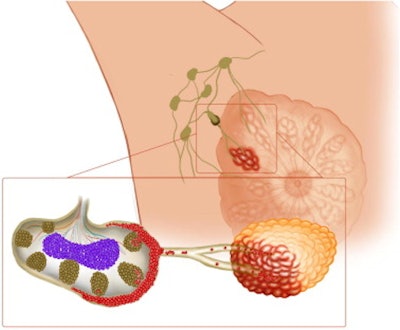 Demonstration of tumoral cells invading the axillary cortex. Images courtesy of Dr. Seda Aladag Kurt and EJR.
Demonstration of tumoral cells invading the axillary cortex. Images courtesy of Dr. Seda Aladag Kurt and EJR.The researchers divided the lymph nodes into three groups depending on the type of cortical thickening as diffuse, closer (eccentric cortical thickening on the side near the tumor and/or breast) and distant (thickening on the further side) asymmetry. For each lymph node, the researchers recorded longitudinal to transverse axis (L/T) ratio, the largest cortical thickness, C/H ratio, hilar status (normal/displaced/absent), orientation (parallel/vertical), capsular integrity (sharp/indistinct), vascularization pattern (hilar/peripheral/penetrant/anarchic/avascular) on superb microvascular imaging (SMI) and presence of conglomeration.
They also recorded axillary nodal status on F-18 FDG PET-CT/MRI scans, if available.
Key findings
A total of 219 metastatic ALNs [diffuse (n = 122), closer asymmetry (n = 71), distant asymmetry (n = 26)] were evaluated. By univariate analysis, ALN metastasis was significantly associated with the presence of closer asymmetrical cortical thickening (p < 0,0001), abnormal vascular pattern (p < 0.001), high C/H ratio (p = 0.001), high, diffuse cortical thickness (p = 0.001), and hilar status (p < 0.005) -- whereby absent or displaced hilus was suspicious for metastasis. By multivariate analysis, nodal metastasis was significantly associated with asymmetrical cortical thickening (p = 0.001), C/H ratio (p = 0.005), and vascular pattern (p < 0.0001).
"In ALNs with asymmetrical cortical enlargement, the side of the thickening (closer or distant asymmetry), the vascular pattern on Doppler [ultrasound], and, if present, the FDG uptake in PET scan, can be used to decide on lymph node sampling," Kurt noted.
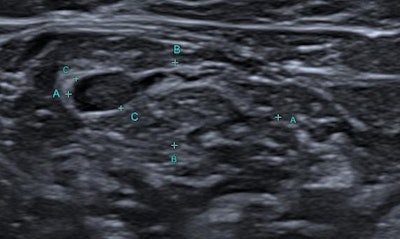 A 58-year-old woman diagnosed as having invasive ductal carcinoma with neuroendocrine differentiation. The lymph node shows asymmetrical cortical enlargement at the closer side to the breast, with remarkable focal abnormal vascularization on SMI (superb microvascular imaging).
A 58-year-old woman diagnosed as having invasive ductal carcinoma with neuroendocrine differentiation. The lymph node shows asymmetrical cortical enlargement at the closer side to the breast, with remarkable focal abnormal vascularization on SMI (superb microvascular imaging).At her institute, radiologists perform an axillary scan in all patients who undergo breast ultrasound and use these findings to decide on sampling lymph nodes or not. An equally important technique for all cases is axillary microvascular imaging using SMI to differentiate benign and malignant axillary lymph nodes.
"Breast radiologists are experienced in ultrasound. But, in my experience there are some tricks about axillary ultrasound that radiologists don't know or use in daily practice," she noted.
The authors concede that further research supported by deep-learning algorithms and with larger sample size is required for the validation of the group's findings.
Screening strategy
In Turkey, the Ministry of Health allows for every woman age 40 and over to be routinely screened with mammography every two years, although the Turkish Society of Radiology recommends annual screening, which is also preferred at Kurt's clinic.
The Ministry's breast cancer screening platform KETEM, was developed through a joint project between Europe and Turkey, in collaboration with the national cancer control program. KETEM comprises mobile mammography units and screening centers operating in public hospitals and health clinics across most towns, to provide a free breast, cervical, and colorectal cancer screening service to patients.
Besides activities related to Pink October, the international breast cancer awareness month, the Turkish government and KETEM work to inform the public about the importance of screening, through social media, TV programs and local government-sponsored events. Such activities form part of a general screening awareness campaign, noted Kurt. In addition, on a smaller scale, some local governments send letters to invite women for screening, but there is not a regular system for doing this, she said.