When physicians craft treatment plans for patients with suspected angina based on cardiovascular MRI (CMR) and SPECT myocardial perfusion imaging (MPI) results, the chance of unnecessary angiographies is much less than if care is based on tried-and-tested guidelines, according to U.K. researchers.
 John P. Greenwood, PhD.
John P. Greenwood, PhD.A review of more than 1,200 symptomatic patients in six imaging centers across the U.K. also found that CMR and MPI were equally as effective in preventing unnecessary angiography at least 12 months after imaging.
Interestingly, the rate of eventual major adverse cardiovascular events and positive angiography outcomes was statistically the same for all three treatment strategies (JAMA, 13 September 2016).
"Some would argue that negative tests are the 'price to pay' for not missing important disease in others," wrote lead author John P. Greenwood, PhD, professor of cardiology and consultant cardiologist at the Leeds Institute of Cardiovascular and Metabolic Medicine, and colleagues. "Avoiding unnecessary invasive angiography could have significant financial benefits, avoids exposing patients to unnecessary risk, and is also a strong patient desire."
Disease prevalence
Coronary heart disease continues to be the leading cause of death and disability around the world, and MPI with SPECT is the most common test worldwide to assess myocardial ischemia. More recently, CMR has gained in popularity due to its noninvasive imaging approach and validated high diagnostic accuracy and prognostic results.
When the two modalities are inconclusive or are unavailable, physicians will turn to invasive coronary angiography to determine the extent of a patient's suspected coronary heart disease. The problem is one recent U.S. study concluded that approximately 60% of elective cardiac catheterizations found no obstructive coronary heart disease.
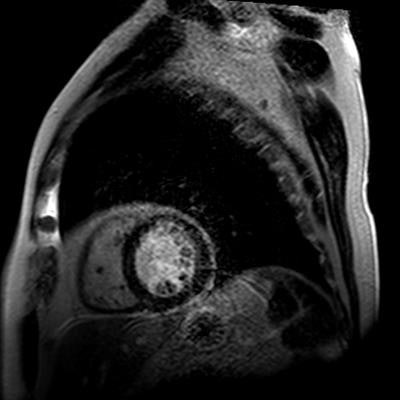
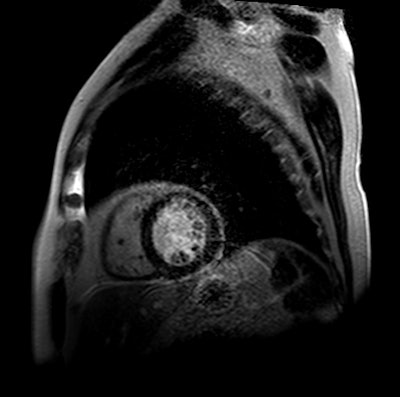
 First-pass stress perfusion CMR image shows hypoperfusion (ischemia) in the septum and anterior wall. Images courtesy of John P. Greenwood. PhD.
First-pass stress perfusion CMR image shows hypoperfusion (ischemia) in the septum and anterior wall. Images courtesy of John P. Greenwood. PhD."Thus, avoiding unnecessary angiography should reduce patient risk and provide significant financial savings," Greenwood and colleagues wrote.
To determine the best strategy to assess high-risk patients with multiple cardiac risk factors, researchers enrolled 1,202 patients from six U.K. imaging centers between November 2012 and March 2015 who fit the study criteria. The mean age of patients, which included 638 men (53%), was 56.3 years (± 9 years).
High-risk patents
All patients were symptomatic for coronary heart disease, with 401 patients (33%) reporting typical chest pain and 801 patients (67%) reporting atypical chest pain as their primary symptom. Subjects also had a pretest likelihood of coronary heart disease ranging from 10% to 90%.
Subjects were excluded if they had no angina, a normal SPECT MPI, or cardiac CT result within the previous two years, a history of a myocardial infarction, previous coronary revascularization, and contraindication to any study noninvasive imaging test.
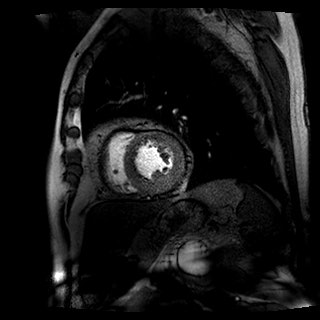
 This CMR image with late gadolinium enhancement shows thin subendocardial scar in the anterior segment.
This CMR image with late gadolinium enhancement shows thin subendocardial scar in the anterior segment.The subjects had median of at least two cardiac risk factors. The detrimental conditions included diabetes (13%), hypertension (38%), past or current tobacco use (58%), high cholesterol (dyslipidemia, 40%), and family history of premature coronary heart disease (54%). All of the patients were candidates for revascularization.
The 1,202 patients then were randomly categorized based on their treatment regimen. There were 240 subjects who followed U.K. National Institute for Health and Care Excellence (NICE) guidelines; 418 cases were directed by CMR results; and 481 individuals whose care was based on MPI findings. Efficacy of the three treatment strategies was determined on unnecessary coronary angiography result within 12 months.
The determination of an unnecessary angiography was based on normal fractional flow reserve of greater than 0.8, coronary angiography showing no percentage diameter stenosis equal to or greater than 70% in one view, or equal to or greater than 50% in two orthogonal views in all coronary vessels no less than 2.5 mm in diameter.
Unnecessary procedures
In reviewing patient outcomes, Greenwood and colleagues found CMR-based care resulted in 36 (7.5%) unnecessary angiographies on symptomatic patients, compared with 34 (7.1%) unneeded procedures in the MPI group (no statistical difference). By comparison, 69 (28.8%) unnecessary angiographies occurred in the NICE guidelines group.
On the other hand, a positive angiography result was observed in 29 patients (12%) in the NICE guidelines group, compared with 47 patients (9.8%) in the CMR group and 42 cases (8.7%) in the MPI group.
A total of 36 patients (3%) reported major adverse cardiac events at follow-up (median of 15.8 months). Of that total, there were six such patients (2.5%) in the NICE group, followed by 15 patients (3.1%) in the CMR group with an adverse cardiac event and similarly 15 patients (3.1%) in the MPI group.
Based on those numbers, researchers concluded there was no statistically significant difference among the three care strategies.
"A CMR-guided strategy significantly reduced unnecessary angiography occurrence compared with NICE guidelines-guided care, but was not significantly different from an [MPI]-guided strategy," the authors concluded.
As an aside, the team did concede there is some debate "as to whether all of unnecessary angiograms in this study were clinically unnecessary," adding that "some would argue that negative tests are the 'price to pay' for not missing important disease in others."