Adding body-coil image acquisition to PET/MRI does not entirely match the diagnostic accuracy of standard low-dose PET/CT, and may only serve as a backup scanning option in a small selection of oncology patients, according to a Swiss study.
The prospective study from University Hospital Zurich also found that more time is needed on the MRI to accommodate breath-holds and additional surface coil sequences to match with the standard low-dose PET/CT (Insights into Imaging, 15 May 2013). Lead author Dr. Philippe Appenzeller is from the division of diagnostic and interventional radiology.
Over the last several years, clinical interest in PET/MRI for oncological imaging has increased, given MRI's ability to image soft tissue and concerns about radiation exposure to patients through PET/CT. However, before PET/MRI can replace PET/CT for some clinical indications, Appenzeller and colleagues noted that MRI is "routinely done with surface coils to achieve sufficient resolution as well as signal density."
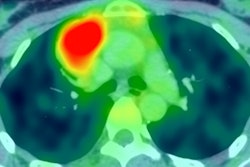
 Comparison of PET/CT and PET/MRI of a patient with diffuse large B-cell lymphoma. Axial CT and MRI images show bulky disease in the mesenterium with corresponding 18F-FDG activity in axial PET/CT and PET/MRI. In this patient, lesion conspicuity was rated as "excellently delimitable" for MRI and "good delimitable" for CT. All images courtesy of Dr. Philippe Appenzeller.
Comparison of PET/CT and PET/MRI of a patient with diffuse large B-cell lymphoma. Axial CT and MRI images show bulky disease in the mesenterium with corresponding 18F-FDG activity in axial PET/CT and PET/MRI. In this patient, lesion conspicuity was rated as "excellently delimitable" for MRI and "good delimitable" for CT. All images courtesy of Dr. Philippe Appenzeller.Even when routine clinical body-coil imaging alone is not adequate to achieve sufficient image quality, there "might be a clinical situation in multimodality imaging where it might be desirable to have a quick whole-body PET/MRI," the authors explained. So, the purpose of their study was to determine the diagnostic utility of a PET/MRI with only an axial T1-weighted fast-gradient-echo sequence using a body coil, which is needed for MRI-based attenuation correction, compared with standard low-dose PET/CT.
Patient cohort
A total of 63 patients with a mean age of 58 (ranging from 19 to 86 years; 23 women, 40 men) referred for either staging or restaging/follow-up of various malignant tumors participated in this prospective study. Sequential PET/CT and MR imaging were performed on a trimodality PET/CT and MRI configuration (Discovery PET/CT 690 and Discovery MR 750, GE Healthcare). The researchers first evaluated PET/CT results and the PET/MRI scans for the presence of PET-positive and PET-negative lesions. Lesions were considered PET-positive if standardized uptake value (SUV) was distinctively greater than the surrounding background activity.
The study used a four-point scale to assess lesion conspicuity. The rating of 1 indicated more than 25% of a lesion's borders could be defined; 2 was used for 25% to 50% of borders depicted; 3 for 50% to 75 % as definable; and 4 indicated more than 75% of a lesion's borders were defined. Additionally, images were divided into three categories: tumor mass, lymph nodes, and lesions. Differences in overall lesion detectability and conspicuity in PET/CT and PET/MRI were investigated, as well as differences in detectability based on the localization and lesion type.
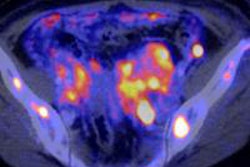
 Comparison of PET/CT and PET/MRI of a patient with a solitary lung metastasis showing superiority of CT versus MRI. Axial CT and axial PET/CT images show the large metastasis in the left lung. The lesion
Comparison of PET/CT and PET/MRI of a patient with a solitary lung metastasis showing superiority of CT versus MRI. Axial CT and axial PET/CT images show the large metastasis in the left lung. The lesion is only detectable in co-registered PET/MRI images but undetectable on the MRI.
The researchers also noted corresponding anatomical structure for each lesion based on the anatomical information of the coregistered PET/CT and PET/MRI image sections.
Common cancers
Of the 63 subjects, the most common ailment was malignant melanoma in 11 individuals (17%), lung cancer in nine cases (14%), breast cancer in seven patients (11%), and Hodgkin's lymphoma among six people (9%). The study was forced to exclude 17 patients from the final analysis, because there were no suspicious tumorous lesions. The remaining 46 participants were examined with sequential PET/CT and MRI and were found to have at least one lesion.
The final analysis included 126 lesions, with 101 lesions (80%) visible and measurable on both PET/CT and PET/MRI. There were 17 lesions (17%) visible only on PET/CT, six lesions (6%) seen only on PET/MRI, and two lesions (2%) not visualized on either CT or MRI.
In addition, 37 (29%) of the 126 PET-positive findings were characterized as tumor mass, 57 (45%) were determined to be lymph nodes, and 17 (13%) were lesions. Overall, 111 PET-positive findings were evaluated because not all PET-positive findings were seen on PET/CT and/or PET/MRI. Of the remaining 15 lesions, FDG-uptake without morphological correlation did not fit in the defined categories.
Statistical significance
The Zurich group found no statistically significant superiority of PET/CT over PET/MRI or vice versa in terms of lesion conspicuity (p = 0.095). There was, however, a statistically significant superiority regarding conspicuity of PET/CT over PET/MRI in pulmonary lesions (p = 0.016), and a statistically significant advantage of PET/CT over PET/MRI in lymph nodes with lesion conspicuity (p = 0.033).
"A higher mean score concerning bone lesions was found for PET/CT compared with PET/MRI," the authors noted. "However, these differences did not achieve statistical significance."
Based on the numbers, Appenzeller and colleagues concluded PET/MRI does not "entirely match the diagnostic accuracy of standard low-dose PET/CT" with body-coil image acquisition.
"One task for the future of PET/MRI, therefore, might be the evaluation of how many MRI sequences and how much information from the MRI is needed (matrix, breath-holds, different weightings) to match up to a standard low-dose PET/CT, ideally within the same acquisition time," they added