Volumetric body composition metrics is a rapidly emerging technique and can be a strong indicator of survival in patients with colorectal cancer (CRC), a study published on 14 June in the European Journal of Radiology has found.
The relationship between the two is complex, however, and conventional approaches may not provide a comprehensive assessment, according to a team from the Departments of Cancer Epidemiology and Breast Oncology at the H. Lee Moffitt Cancer Center & Research Institute in Tampa, Florida, U.S.
While obesity increases the risk of developing CRC, patients with higher BMIs at diagnosis have been shown to have lower mortality rates than those with lower BMIs. The relationships have been shown to be dependent on the distribution and proportions of skeletal muscle (SM), visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), and intermuscular adipose tissue (IMAT).
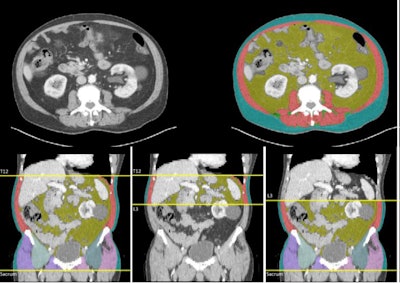 Examples of CT volumetric and single-slice images produced by Data Analysis Facilitation Suite (DAFS) v3.9 software are displayed.Figure courtesy of Dr. Daniel Jeong and EJR.
Examples of CT volumetric and single-slice images produced by Data Analysis Facilitation Suite (DAFS) v3.9 software are displayed.Figure courtesy of Dr. Daniel Jeong and EJR.
The single-slice CT analysis of the mid-third lumbar (L3) vertebral axial that is commonly used for this analysis, while consistent, has the limitation of not capturing the variable distribution of abdominal fat and muscle.
To determine if volumetric analysis would produce a more complete assessment of body composition in CRC patients, the researchers performed a study in which they investigated the potential associations between volumetric body composition metrics and all-cause survival among newly diagnosed pretreatment CRC patients compared with single-slice body composition metrics.
The study cohort comprised ColoCare Study participants enrolled from the Moffitt Cancer Center between December 2009 and August 2023 with available pretreatment abdomen through pelvis CT scans with intravenous contrast. It included patients 18 or older who have been newly diagnosed with primary invasive CRC (stages I-IV), have no prior history of cancer, and who are undergoing surgery, as close to their CRC diagnosis as possible.
The mean age at diagnosis was 61, and the sample was nearly evenly split between men and women. The cohort was predominantly white (94%); most participants had a BMI of 25 or higher (78%). There were also near-even numbers of those diagnosed with colon or rectum tumors. Nearly all patients were treated with surgery (92%); 34 (28%) received only surgery; 32 (26%) received surgery and chemotherapy; 42 (35%) received surgery, chemotherapy, and radiation; and 45 (37%) patients received neoadjuvant therapy.
The authors, led by radiologist Dr. Daniel Jeong, used three boundaries to estimate muscle and fat distribution for the volumetric body composition metrics: the total (T12-sacrum), upper abdomen (T12-L3), and lower abdomen/pelvis (L3-sacrum). They noted that the upper and lower abdominal metrics were evaluated separately because fat and muscle compartments are not evenly distributed across the abdomen, and region-specific metrics may provide refined, more-specific information. All output was reviewed by a board-certified abdominal radiologist with several years of experience to ensure accurate segmentation analysis.
Complete pretreatment T12-sacrum CT images and covariate information from a total of 121 participants were included in the analysis, of whom 38 (31%) died within a mean follow-up period of 7.7 years (range, 0.7-13.8). Those who died were older at diagnosis (66 years vs. 58 years, p = 0.004) and more likely to be diagnosed with stage IV disease (p = 0.05) than those who survived the study period.
In fully adjusted models, higher T12-sacrum and L3-sacrum VAT/SAT index ratios were significantly associated with poorer CRC survival (T12-sacrum, hazard ratio [HR]: 1.66, 95% confidence interval [CI]: 1.01, 2.72, p = 0.05; L3-sacrum, HR: 1.8, 95% CI: 1.13, 2.87, p = 0.01). For the single-slice analysis, the mid-L3 VAT/SAT ratio was also statistically significantly associated with worse CRC survival (HR: 1.58, 95% CI: 1.01, 2.47, p = 0.05). The T12-sacrum and L3-sacrum CRC survival associations did not differ significantly from the mid-L3 association, and all volumetric VAT/SAT index ratios were highly correlated with the mid-L3 metric.
The researchers added that there was evidence that the volumetric VAT/SAT ratio measured from L3-sacrum had stronger survival associations than the mid-L3 VAT/SAT ratios, but that they did not reach statistical significance.
However, they concluded that the findings “reinforce the importance of abdominal adiposity distributions in CRC survivorship,” as well as demonstrating that volumetric body composition metrics could provide new prognostic information about CRC survival.
Read the full study here.