Two major reports published today by the U.K. Royal College of Radiologists (RCR) reveal the true scale of the workforce problems facing the National Health Service (NHS) and the ever-greater reliance on outsourcing. Unless urgent action is taken, patient delays will worsen, with staff pushed to breaking point, the RCR warns.
The pressures of chronic staff shortages are causing a retention crisis, with the most experienced staff now leaving younger than ever before, according to the RCR. In 2024, the median age of consultant clinical radiologists leaving the NHS workforce was 50 (down from 55 in 2020), and 40% of leavers were younger than 45.
“This year’s clinical radiology (CR) census once again lays bare the scale of the challenge we face, with chronic problems such as workforce shortages, reporting backlogs, and staff vacancies remaining too high,” wrote Dr. Robin Proctor, RCR’s medical director for professional practice (CR), in the foreword to the CR report. “Whilst this report rightly makes the case for urgently needed workforce growth, we also need to think about how we make best use of our consultant radiologists. The system is not currently enabling us to work at our best -- indeed, it is actively driving many of us away.”
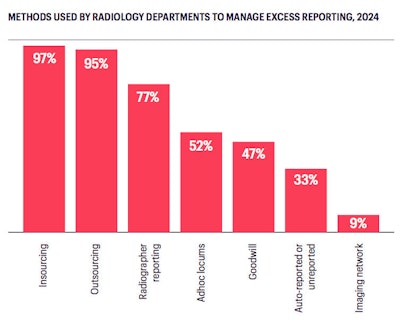
For the first time, no radiology department in the U.K. met its reporting requirements within staff contracted hours, according to the RCR. The prevalence of both insourcing (paying staff overtime) and outsourcing (paying teleradiology companies to conduct some reporting) rose to 97% and 95%, respectively. Larger radiology departments rely more heavily on insourcing (100% use this method), whereas smaller departments rely more heavily on outsourcing (95% use this method).
 All figures courtesy of the RCR.
All figures courtesy of the RCR.
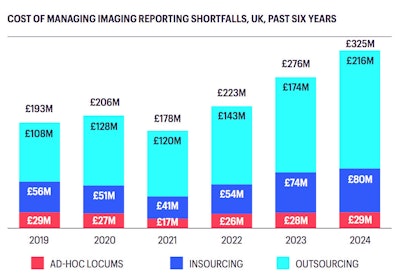
In 2024, NHS trusts and health boards spent £325 million on insourcing and outsourcing. This represents a 16% increase over 2023 expenditure and is equivalent to the cost of 2,910 CR consultant salaries. The RCR forecasts an expenditure of £547 million in five years’ time if current trends continue.
The bulk of this expenditure goes towards outsourcing, which rose by over £42 million between 2023 and 2024, the RCR noted. At the time of writing, there were over 600 radiology consultants on the General Medical Council (GMC) register whose designated body (typically, a doctor’s primary employer) was a teleradiology company. In October 2023, the U.K. had 4,624 clinical radiologists working in the NHS, including consultants and specialty and associate specialist (SAS) doctors. Also, there were 2,049 radiology doctors in training.
There were approximately 200 radiologists who had their designated body as a teleradiology company and who no longer appear in the RCR census data, implying they work almost exclusively in teleradiology, the report said. “This is a small fraction of all those who do some teleradiology work, most of whose designated employers are NHS trusts/health boards. Nonetheless, there is some degree of ‘loss’ from the NHS to the teleradiology sector, though it is difficult to quantify.”
The prevalence of less than full-time (LTFT) working rose to 39% in 2024, continuing the trend seen in previous years. LTFT working is most common among older CR consultants -- 26% of those under the age of 40 work LTFT, compared with 41% of those aged 50-59 -- but prevalence has risen across all age groups over the past six years.
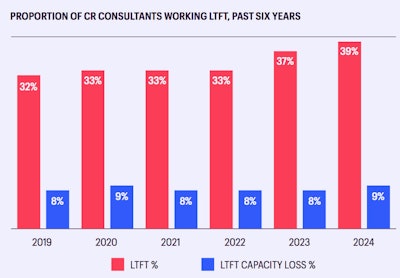
Many people use this time for education or research, for childcare or other family commitments, or for wellbeing reasons, but the RCR conceded that some may be opting for LTFT in order to work part-time for a teleradiology company.
Other trends identified in the report include the following:
- In 2024, 56% of clinical directors reported no significant change to their workloads from adopting AI tools, and 37% reported an increase in their workload directly as a result of implementing and/or using AI tools. These figures exclude the 30% of clinical directors who reported not using AI tools.
- Excluding general radiologists, the groups with the highest forecast retirement rates are chest/lung radiology (26% within five years), cancer imaging (26%), and breast radiology (22%). Breast radiology has seen a 4.8% average annual attrition over the past five years (vs. 3.8% averaged across all special interests), compared to 1.4% for cardiac radiology. Other special interests with higher relative attrition rates are musculoskeletal (3.5%) and radionuclide imaging (4.6%).
- Over the past five years, uroradiology has grown by 8.3%, cardiac radiology by 7.4%, head and neck radiology by 7.1%, and gastrointestinal radiology by 6.7%.
- 42% of diagnostic CR consultants are women. Over the past decade there has been a gradual increase in the proportion of CR consultants (diagnostic and interventional) who are women, from 33% in 2015 to 37% in 2024, but only 12% of interventional radiology (IR) specialists are women.
- In 2024, 344 people started CR specialty training and 265 completed their training. CR specialty training residents comprise 29% of the total CR workforce. Over the past five years, there has been an average annual increase in radiology resident headcount of 4.8%, but some areas have seen little or no growth (e.g., Northern Ireland 0.4%, North and West Wales 1.9%). In south-east Scotland, the resident cohort has shrunk by an average of 3.7% each year since 2019.
- 83% of clinical directors said they lacked sufficient radiographers to operate any new scanners, and 72% said they lacked sufficient radiologists to report on the images it would generate. 53% indicated they lacked sufficient space to house an additional scanner.
The McCoubrie viewpoint
NHS radiology has never faced such a crisis, Dr. Paul McCoubrie, a consultant radiologist at Southmead Hospital in Bristol, told AuntMinnieEurope. “It’s little wonder that radiologists are fleeing the NHS -- younger ones emigrating or working for lucrative teleradiology companies, and older radiologists retiring as soon as financially possible.”
The RCR has been warning about workforce shortages for nearly three decades, documenting the problems and accurately predicting the future, he continued. “The RCR has been insistent but reasonable over the years and consequently has been ignored by government and NHS higher echelons. And like Cassandra, they speak the truth but seem doomed to be ignored.”
McCoubrie said he can’t understand why successive governments and NHS leaders have not taken the RCR’s warnings seriously. “It isn’t that the data isn’t good; it’s highly representative. It isn’t that the RCR hasn’t shouted loud enough; they most certainly have. I suspect it is because, like it or not, radiology is a Cinderella specialty: underappreciated, underfunded, and generally neglected as a specialty. Like geriatrics and psychiatry, radiology is not seen as frontline, sexy or important.”
He thinks three vital questions remain unanswered: Will radiology get to go to the ball? Will we see a big uptick in the number of radiology resident doctors? Will we get funding to meet demand? “I wouldn’t hold your breath. NHS finances are parlous, and many specialties have shortages. Not quite as bad as radiology and not for quite as long. I cannot see Wes Streeting (Secretary of State for Health and Social Care) advancing to the west side of Lincoln’s Inn Fields with a glass slipper anytime soon.”
It’s time for the RCR to take the gloves off and start using stronger media tactics, McCoubrie added. “The RCR has been positioning itself as the Royal College of cancer for some time. They also do this as they know they’ll get headlines and more reliable media exposure. This is crucial when you are dealing with populist governments. They respond to headlines and media hype, not logic and reason ... The RCR has to play a little dirty, otherwise radiology and oncology in this country is doomed.”
Frustration over MDTs
As it becomes ever clearer that radiologist numbers will never catch up with the rising demand for services, the focus is shifting more towards working out how to make the best use of existing staff, another expert source told AuntMinnieEurope.
“One of the growing demands highlighted in the report is the time spent on multidisciplinary team meetings (MDTs, or tumour boards),” the source said. “Radiologists value these opportunities to witness directly the impact of our interpretations on patient management, but there is increasing frustration at the apparent inefficiency in the conduct of many such meetings.”
For example, a radiologist might spend considerable time reviewing images in advance of the meeting, only to find that certain patients are not discussed that week but deferred to another occasion when another radiologist will repeat the exercise, according to the expert.
“More time spent in meetings means less time for reporting and helps to drive the remarkable rise in NHS spend on outsourced reporting, which is on course to more than double in the five years from 2021 to 2026,” the source added. “The extent of the ‘loss’ of radiologists from the public sector to the private teleradiology sector is something highlighted for the first time in this year’s report.”
The lack of women in IR has been a concern for some time and doesn’t yet seem to be improving, the expert noted. “The 7.9% increase in interventional neuroradiologists in the past five years is nothing like enough to support the demand for mechanical thrombectomy in stroke.”
For more details on the 2024 radiology and oncology workforce reports and to download free copies of both documents, go to the RCR website.




















