The use of spectral CT is rising, but its clinical integration and quality assurance (QA)/quality control practices are inconsistent, an International Atomic Energy Agency (IAEA) survey of medical physicists, radiologists, and medical radiation technologists has found.
Standardized protocols, targeted training, and international guidance are urgently needed to support the safe and effective adoption of spectral imaging, according to the survey team led by Virginia Tsapaki, PhD, a medical physicist at the IAEA's Dosimetry and Medical Radiation Physics section in Vienna.
More than half of the 91 responses came from European and Asia-Pacific nations. The authors' findings, published 16 October in Insights into Imaging, indicate increasing awareness and prioritization of diagnostic imaging capabilities, even in settings with limited resources.
"Specifically for Africa, it is noteworthy that responses were received from countries that are not traditionally among the largest or most resourced in terms of medical technology infrastructure; notably, countries like Niger, Rwanda, and Senegal, indicating interest in advanced CT technology even in settings not traditionally seen as high resource," they pointed out.
However, clinical adoption of spectral CT remains fragmented overall and highly dependent on local protocols and vendor-specific capabilities, the researchers added. Their online survey, conducted between October 2024 and June 2025, revealed why spectral CT is not routinely used, elaborating on five key issues:
- Clinical relevance and demand
- Knowledge and training barriers
- Technical and workflow limitations
- Operational and administrative barriers
- Variation in use and access
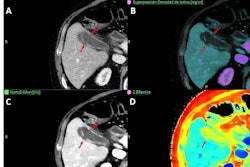
In some settings, spectral CT was only employed for very specific applications, such as cardiac imaging or oncology, while other departments relied entirely on conventional single-energy CT. Several respondents noted that while spectral CT provides extra data (such as perfusion maps or virtual noncontrast images), the information is not always considered clinically useful or relevant, leading to limited utilization, Tsapaki and colleagues noted.
A majority of those who responded were medical physicists. Radiologists made up 8%, while 18% were medical radiation technologists. In addition, a diversity of scanning systems (Siemens Healthineers, GE HealthCare, Canon Medical Systems, and Philips) were represented.
Importantly, in 40 of the responding institutions, radiologists had received some spectral CT training, whereas in 24 institutions, radiologists received no training at all, and 19 did not provide any response, the authors found. A similar pattern was observed for medical radiation technologists. In contrast, medical physicists showed a lower number of trained individuals, with 40 reporting no training and 19 not responding, according to the findings.
A technical and workflow limitation cited is the prescan requirement to decide prospectively whether to use spectral imaging. This adds complexity to the workflow and may discourage routine use, especially in high-throughput settings, the group noted.
Despite the challenges, the most common spectral CT clinical applications appear to be pulmonary embolism, especially in older patients or those requiring reduced contrast due to renal impairment, the survey highlighted. Abdominal imaging was frequently mentioned, often for lesion characterization, perfusion analysis, or low-contrast-dose studies.
Several sites also reported cardiac or oncologic imaging, musculoskeletal assessments, and routine radiation therapy planning, particularly for head, neck, prostate, and spine. Moreover, some sites are using spectral CT for stroke assessment and postoperative brain scans, as well as differentiating hemorrhage from contrast, according to the findings.
"Our results also echo concerns raised in the literature about the variability introduced by differences in hardware and post-processing algorithms across CT vendors," the authors wrote.
Variability underscores the importance of context-specific strategies to support adoption -- such as tailored clinical guidelines, case-based learning, and evidence generation through multicenter studies, they added.
Notably, 53% of facilities were not performing dedicated quality control testing, and 61% of facilities reported that their dosimetry practices remain unchanged, the group found, noting the need for clearer guidance and standardization in both QA and dosimetry practices.
The survey focused heavily on technical aspects of spectral CT, recording inventory and capability, followed by detailed QA information, dosimetry practice, and technical protocol use.
Read the complete survey results, including the proportion of weekly CT examinations performed using spectral imaging across surveyed scanners, here. The co-authors were Zoe Brady, Nathaly Barbosa, Marc Kachelrieß, Mahadevappa Mahesh, Egor Titovich, Bronwin Van-Wyk, and Mauro Carrara.