In what is sure to be a controversial study among cancer screening advocates, researchers from Norway have concluded that screening mammography and CT for lung cancer screening don't necessarily extend patients' lives, according to results published on 28 August in JAMA Internal Medicine.
Although researchers led by Dr. Michael Bretthauer, PhD, from the University of Oslo do not advocate for cancer screening tests to be abandoned, they suggest that claims of screening saving lives are not supported by the "current best available evidence."
"It might be wise to reconsider priorities and dispassionately inform interested people about the absolute benefits, harms, and burden of screening tests that they consider undertaking. Our estimates may serve that purpose," Bretthauer and colleagues wrote.
Proponents of regular cancer screening contend that these exams save lives by reducing mortality rates. However, the researchers noted that it's not known if people will live longer if they undergo common cancer screening tests.
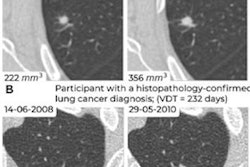
Bretthauer and colleagues sought to calculate the association between several cancer screening tests and life days gained. They did so by gathering data from large-scale randomized clinical trials with long-term follow-up. They analyzed the following tests: mammography; low-dose CT screening for smokers and former smokers; colonoscopy; sigmoidoscopy, or fecal occult blood testing (FOBT) for colorectal cancer; and prostate-specific antigen (PSA) testing for prostate cancer.
The researchers included data from 2.1 million individuals enrolled in 22 randomized clinical trials. Median follow-up was 10 years for CT, PSA testing, and colonoscopy; 13 years for mammography; and 15 years for sigmoidoscopy and FOBT.
The team found that sigmoidoscopy was the only screening test with statistically significant life days gained at 110 days, with a range of zero to 274 days. Mammography led to zero days gained, with a range of between -190 to 237 days. While CT lung cancer screening led to 107 days gained on average, the range was between -286 days to 430 days, according to the researchers. For all other tests, overall gains ranged from zero to 37 days.
However, the studies selected varied by publishing dates. For example, two mammography screening studies used for the study were published in 1989. Another was from 2014. For FOBT, the studies used were published between 1999 and 2012.
The study authors suggested that the lack of increased longevity could be due to competing causes of death, such as other diseases, accidents, suicides, and incidental diseases from surveillance and screening, among others.
While the researchers noted that cancers detected and treated at an early stage can prevent cancer-related death at a younger age, they also suggested that people can experience a lifetime loss due to screening-related harms.
The authors suggested that it could be worthwhile to implement screening tests with a positive benefit-harm balance measured in incidence and mortality of the target cancer compared with harms and burden.
"However, organizations, institutions, and policymakers who promote cancer screening tests by their effect to save lives may find other ways of encouraging screening," they wrote.
In an accompanying editorial, Dr. H. Gilbert Welch and Tanujit Dey, PhD, from Brigham and Women's Hospital in Boston wrote that while it's not feasible to test all-cause mortality when screening for an individual cancer, multicancer screening could be a more efficient method.
"Observational data on the effects of cancer screening are misleading. Multicancer screening would entail tremendous costs and potentially substantial harms," they wrote. "For these reasons, a randomized clinical trial is mandatory not only to learn if multicancer screening saves lives but also to learn how frequently it causes harm."
The full study can be found here.