PET/MRI is a promising tool in the pre-therapeutic assessment of primary tumors of the upper aerodigestive tract with lymph node extension, particularly in the identification of predictive characteristics of recurrence or progression, a leading French research group has reported.
"Lymph node PET/MR analysis has shown that the strongest predictors of recurrence were lymph node enhancement and SUVmax for the contralateral nodes and enhancement, SUVmax node shape for the homolateral nodes," noted Dr. Nadya Pyatigorskaya, PhD, a neuroradiologist at the Pitié-Salpêtrière University Hospital (l'Assistance publique - Hôpitaux de Paris, AP-HP) in Paris and a researcher in the MOV'IT multidisciplinary team at the Paris Brain Institute, and colleagues.
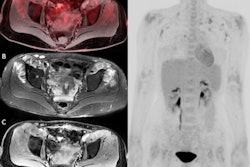
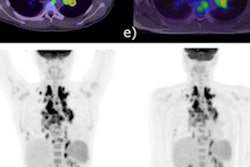
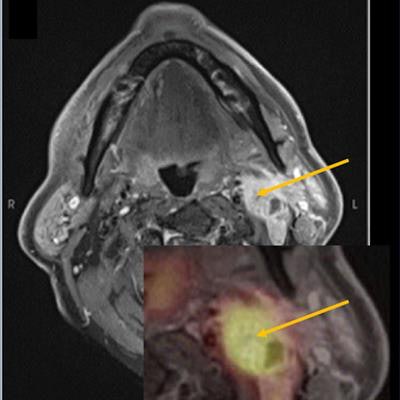
 Metastatic lymph nodes in head and neck squamous cell carcinoma with contrast enhancement and high standardized uptake value (SUV). Figure courtesy of Dr. Nadya Pyatigorskaya, PhD, and presented at ISMRM 2023.
Metastatic lymph nodes in head and neck squamous cell carcinoma with contrast enhancement and high standardized uptake value (SUV). Figure courtesy of Dr. Nadya Pyatigorskaya, PhD, and presented at ISMRM 2023.Cancers of the upper aerodigestive tract mostly consist of head and neck squamous cell carcinomas (HNSCCs), which account for 90% of stage I head and neck cancers and represent the sixth most common cancer worldwide. HNSCC have a high recurrence rate and represent one of the most common histological types to metastasize to regional lymph nodes, Pyatigorskaya explained in an e-poster presentation on 7 June at the International Society for Magnetic Resonance in Medicine (ISMRM) meeting in Toronto.
"Metastatic nodes are mostly homolateral to the primary tumor, but contralateral or bilateral nodes are not rare, especially when the primary tumor is medial or posterior," she stated. "The risk of lymph node metastasis occurs for the largest tumors, mostly T3-T4. The presence of metastatic nodes reduces significantly the five-year survival rate."
Lymph nodes are generally assessed by CT and MRI, mostly based on size and some morphology criteria with a lack of specificity, but F-18 FDG PET and advanced MRI methods, such as dynamic MRI and diffusion-weighted imaging (DWI), are also useful for detection of lymph node metastases.
While homolateral lymph nodes are usually resected, contralateral nodes are resected only if invasion is strongly suspected, according to Pyatigorskaya. "In this context it is extremely important to detect on the baseline imaging the signs of contralateral node invasion for the correct management."
Study logistics
A total of 273 consecutive patients with histopathologically confirmed upper aerodigestive tract cancer who underwent PET-MRI at the Pitié-Salpêtrière between 2015 and 2020 were retrospectively included in the study.
For each patient, the histological type of tumor and the presence of active smoking and chronic alcoholism -- and for cases of recurrence, the location of the recurrence -- were recorded. The patients were divided into two groups: a case group (subdivided into two subgroups: recurrence and progression) and a control group, represented by patients having a primary tumor with lymph node extension but no recurrence after management.
The examinations were performed on PET/MRI scanner (Signa 3-tesla from GE HealthCare), 60 minutes after injection of 3 to 5 MBq/kg of F-18 FDG. The MR sequences included axial T2 (IDEAL) fast-spin echo (FSE), axial T1 FSE, DWI, arterial spin labeling (ASL), 3D T1 FSE after fat saturation, and injection of gadoterate meglumine.
The PET exam was performed simultaneously with a 256x256 array on the head and neck and lasted 16 minutes, followed by a simultaneous whole-body PET/MRI acquisition from the neck to the proximal femurs, including four 192x192 arrays on the rest of the body, accompanied by a T1 lavaflex MRI sequence on the whole body.
Two radiologists analyzed each lymph node aspect and measured the size and quantitative, and cellularity and the vascularization represented by DWI (apparent diffusion coefficient, ADC) and ASL analysis (cerebral blood flow). The semiquantitative SUVmax was measured by nuclear physicians experienced in head and neck imaging. The analysis was performed on an Advantage Workstation (AW4.6, GE HealthCare).
For the lymph nodes contralateral to the tumor, multiple correspondence analysis revealed three dimensions that explained 71% of the total variance, the authors pointed out. In this analysis, the semiological signs -- including lymph node enhancement, disappearance of the hilum of the lymph node, and SUVmax -- appeared to be statistically discriminating between the "control" and "case" groups.
For the lymph nodes homolateral to the tumor the parameters discriminating the control and case groups in at least one dimension included central necrosis, lymph node margins, blurred margins disappearance of the hilum, enhancement, whether intense and homogeneous or intense and heterogeneous SUVmax > 6, the lymph node shape, whether it is rounded or spiculated, periganglionary fat, infiltrated.
The criteria of lymph node enhancement, SUVmax, and lymph node shape were the most discriminating, as they represent a high percentage in two dimensions, as shown in the overall analysis.
"In lymph node PET/MR analysis in HNSCC tumors, the strongest predictors of the recurrence were lymph node enhancement, disappearance of the ganglionic hilum, and SUVmax for the [contralateral] and lymph node enhancement, SUVmax and the lymph node shape for the homolateral nodes," the authors wrote. "Interestingly, size, ADC, and regional cerebral blood flow were not predictors of recurrence."
Future directions
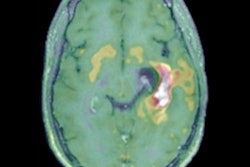
Pyatigorskaya is now focusing her efforts on the development of PET/MRI studies to improve the diagnosis, prognosis, and understanding of neurodegenerative diseases and brain tumors, she noted in an article posted by Institut de Cerveau on 19 December 2022.
"I am particularly interested in progressive supranuclear palsy (PSP)," she said. "Thanks to an industrial collaboration, we have access to a very specific marker of Tau proteins, which accumulate pathologically in the brain of patients. Our goal is to better diagnose and understand the pathological mechanisms of the different forms of PSP."
Today, the more classic forms of PSP, such as Richardson's syndrome, are fairly easy to diagnose in their advanced forms, but in 60% to 70% of cases, they are atypical forms, which are much more difficult to detect, she added. "This is very important. Currently, these patients with atypical forms are not included in clinical trials because their disease is not well understood. In the early forms, the correct diagnosis is also often difficult to make, so it is necessary to improve it."
In terms of abnormal movements, Pyatigorskaya hopes to apply technological developments to therapeutic trials. "Neuromodulation also seems to me to be very promising for modulating the activity of deep brain regions in a non-invasive way, with many potential therapeutic indications such as epilepsy, certain psychiatric disorders, pain or brain tumors."
The co-authors of the ISMRM 2023 study were Drs. Yoann Sclover, Aurelie Kas, Lydia Yahia-Cherif, and Melika Sahli Amor.