Endoscopic ultrasound can avoid the need for confirmatory mediastinoscopy after negative systematic findings in patients with resectable non-small cell lung cancer (NSCLC), according to research published on 5 April in the Journal of Clinical Oncology.
Researchers led by Dr. Jelle Bousema from Máxima Medical Center in Eindhoven, the Netherlands, found that leaving out confirmatory mediastinoscopy and proceeding to immediate lung tumor resection resulted in only a small unforeseen N2 rate -- cancer in the lymph nodes -- after definite surgical lung tumor resection.
"Implementation of the current findings prevents patients from morbidity of confirmatory mediastinoscopy, it reduces the lung cancer staging period, and it probably saves health care costs," Bousema and co-authors wrote.
There is debate among researchers about the value of confirmatory mediastinoscopy after tumor-negative findings on endoscopic ultrasound. This is done as part of mediastinal staging in patients with resectable NSCLC and who have a high probability of mediastinal nodal involvement. Critics say mediastinoscopy has a limited nodal metastasis detection rate, has associated morbidity, and can delay the start of lung cancer treatment.
The researchers noted that the effect of leaving mediastinoscopy out of the process has not been explored in a randomized setting. Previous studies also suggest that endoscopic ultrasound has high sensitivity in this application.
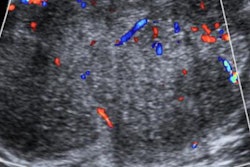
Bousema et al wanted to find out if endosonography alone is enough for effective mediastinal staging in patients with resectable NSCLC. They looked at data from 360 patients with suspected resectable NSCLC and an indication for mediastinal staging after negative systematic endosonography. The patients were randomly assigned to immediate lung tumor resection (n = 178) or confirmatory mediastinoscopy followed by tumor resection (n = 182).
The researchers used a noninferiority margin of 8% that previously showed to not compromise survival. They used the presence of unforeseen N2 disease after tumor resection with lymph node dissection as a primary outcome.
The team reported that mediastinoscopy detected metastases in 8.0% of patients. They also found that unforeseen N2 rate after immediate resection was noninferior at 8.8% compared with mediastinoscopy first (7.7%) in both intention-to-treat (pnoninferior = 0.0144) and per-protocol analyses (pnoninferior = 0.0157).
Confirmatory mediastinoscopy reduced the unforeseen N2 rate by just 1.03%. The researchers wrote that this came at the expense of 10-day delay for lung tumor resection, morbidity in 6.3%, mortality in 0.6%, and repeat general anesthesia in all patients involved. Additionally, major morbidity and 30-day mortality was 12.9% after immediate resection versus 15.4% after mediastinoscopy first (p = 0.4940).
The study authors suggested that based on their findings, confirmatory mediastinoscopy after negative systematic endoscopic ultrasound can be left out for these patients.