CT-guided pulsed radiofrequency combined with steroid injection appears promising for relieving pain in patients with lumbar disk herniation, according to a study published on 28 March in Radiology.
In a clinical trial, an international group led by researchers at Policlinico Umberto I -- Sapienza University of Rome found the combined procedure provided more effective pain relief and disability improvement in patients than standard transforaminal epidural steroid injection (TFESI) alone. The approach could ultimately reduce the need for more invasive treatments, the group suggested.
"The results of our trial demonstrate that a combined treatment of pulsed radiofrequency and TFESI leads to better outcomes at one year following a single 10-minute procedure," said lead author Dr. Alessandro Napoli, PhD, in a news release from RSNA.
Among available options for patients with sciatic pain due to lumbar disk herniation, transforaminal epidural steroid injection (TFESI) is the only interventional procedure recommended in clinical guidelines for patients. However, the duration of benefit is usually short, and additional treatments are often necessary, including surgery.
Pulsed radiofrequency (PRF) is an emerging minimally invasive procedure for relieving sciatica pain. PRF is a modification of radiofrequency ablation in which pulses of high-frequency energy from a probe are applied directly to nerve roots near the spine. This reduces pain signals to the brain.
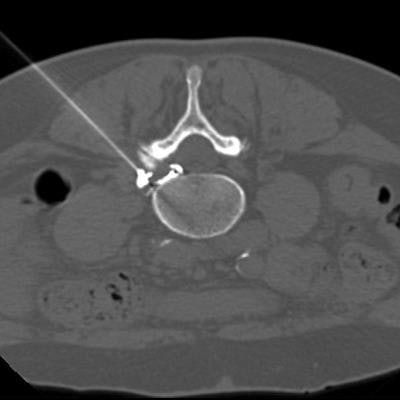
![CT-guided pulsed radiofrequency (PRF) with transforaminal epidural steroid injection. A 62-year-old woman underwent PRF followed by transforaminal epidural steroid injection for sciatica due to left contained intraforaminal disk herniation at the L4-5 level. (A) A 22-gauge needle electrode with a 10-mm active tip was introduced and advanced using one 3-mm oblique axial unenhanced CT scan, which revealed that the needle tip was proximate to the target dorsal root ganglion with the lateral foraminal portal of entry. (B) Sensitive stimulation (50 Hz) PRF current with a threshold of no more than 0.2 V was used to confirm proper positioning by evoking tingling or electric pain in the dermatome that had to match the target dorsal root ganglion. Therapeutic PRF was then performed in one 10-minute session with E-dose functionality, maintaining temperature below the threshold for neural damage (42°C) and a constant voltage (45 V) (G4 RF Generator; Boston Scientific). Immediately after PRF administration, epidural spread of 0.3 mL of contrast material (350 mg of iodine per milliliter, Iomeron; Bracco) was confirmed using intermittent intraprocedural CT fluoroscopic imaging with no intravascular contrast material flow demonstration. A combination of steroid and anesthetic (1 mL lidocaine [ 20 mg/mL] and 2 mL dexamethasone [10 mg/mL]) was then injected without altering needle position to conclude the procedure. Image and caption courtesy of Radiology.](https://img.auntminnieeurope.com/files/base/smg/all/image/2023/04/ame.2023_03_27_20_38_2237_2023_03_28_prf_version2.png?auto=format%2Ccompress&fit=max&q=70&w=400) CT-guided pulsed radiofrequency (PRF) with transforaminal epidural steroid injection. A 62-year-old woman underwent PRF followed by transforaminal epidural steroid injection for sciatica due to left contained intraforaminal disk herniation at the L4-5 level. (A) A 22-gauge needle electrode with a 10-mm active tip was introduced and advanced using one 3-mm oblique axial unenhanced CT scan, which revealed that the needle tip was proximate to the target dorsal root ganglion with the lateral foraminal portal of entry. (B) Sensitive stimulation (50 Hz) PRF current with a threshold of no more than 0.2 V was used to confirm proper positioning by evoking tingling or electric pain in the dermatome that had to match the target dorsal root ganglion. Therapeutic PRF was then performed in one 10-minute session with E-dose functionality, maintaining temperature below the threshold for neural damage (42°C) and a constant voltage (45 V) (G4 RF Generator; Boston Scientific). Immediately after PRF administration, epidural spread of 0.3 mL of contrast material (350 mg of iodine per milliliter, Iomeron; Bracco) was confirmed using intermittent intraprocedural CT fluoroscopic imaging with no intravascular contrast material flow demonstration. A combination of steroid and anesthetic (1 mL lidocaine [ 20 mg/mL] and 2 mL dexamethasone [10 mg/mL]) was then injected without altering needle position to conclude the procedure. Image and caption courtesy of Radiology.
CT-guided pulsed radiofrequency (PRF) with transforaminal epidural steroid injection. A 62-year-old woman underwent PRF followed by transforaminal epidural steroid injection for sciatica due to left contained intraforaminal disk herniation at the L4-5 level. (A) A 22-gauge needle electrode with a 10-mm active tip was introduced and advanced using one 3-mm oblique axial unenhanced CT scan, which revealed that the needle tip was proximate to the target dorsal root ganglion with the lateral foraminal portal of entry. (B) Sensitive stimulation (50 Hz) PRF current with a threshold of no more than 0.2 V was used to confirm proper positioning by evoking tingling or electric pain in the dermatome that had to match the target dorsal root ganglion. Therapeutic PRF was then performed in one 10-minute session with E-dose functionality, maintaining temperature below the threshold for neural damage (42°C) and a constant voltage (45 V) (G4 RF Generator; Boston Scientific). Immediately after PRF administration, epidural spread of 0.3 mL of contrast material (350 mg of iodine per milliliter, Iomeron; Bracco) was confirmed using intermittent intraprocedural CT fluoroscopic imaging with no intravascular contrast material flow demonstration. A combination of steroid and anesthetic (1 mL lidocaine [ 20 mg/mL] and 2 mL dexamethasone [10 mg/mL]) was then injected without altering needle position to conclude the procedure. Image and caption courtesy of Radiology.Evidence to support the combined approach of these procedures is lacking, according to Napoli and colleagues. In this study, the researchers hypothesized that combining PRF and TFESI would be more effective than TFESI alone.
The group enrolled a total of 351 participants (223 men) with sciatica. Patients were randomly assigned to receive a single CT-guided pulsed radiofrequency treatment combined with TFESI (174 patients) or TFESI alone (177 patients). All procedures were carried out in an outpatient clinic, took only 10 minutes, and were performed without general anesthesia, the authors wrote.
At four, 12, and 52 weeks, there was greater leg pain reduction and greater disability improvement in participants who received PRF combined with TFESI compared with the participants who only received the steroid injection.
| Outcomes at 1 year for sciatica pain relief | ||
| TFESI group | Combined PRF and TFESI group | |
| Pain improvement | 69% | 96% |
| Complete pain reduction | 13% | 68% |
"Pulsed radiofrequency combined with transforaminal epidural steroid injection is more effective for pain relief and disability improvement than steroid injection alone," Napoli and colleagues wrote.
In an accompanying editorial, Dr. Jack Jennings, PhD, of the Washington University Mallinckrodt Institute of Radiology in St. Louis, Missouri, U.S., wrote that the study results are promising and that PRF may become another tool in the armamentarium for treating individuals with chronic sciatic pain.
"Further studies on the long-term benefits, cost-effectiveness, and comparison to minimally invasive disk surgery will help to further stratify its role in the treatment of this often morbid, debilitating, and challenging condition," Jennings concluded.



















