How do forensic radiologists perform and report postmortem CT scans? What practical problems and issues do they face when scanning a deceased person? What is the psychological toll of postmortem reporting?
To answer these and other questions, the RadCast team recently spoke with Dr. Peter Kralt and Dr. Lenetta Boyce, who report postmortem CT (PMCT) imaging for the U.K.-based digital autopsy company iGene. Established in 2011, the company has developed its own proprietary imaging software for use with a CT scanner to help determine cause of death and avoid the need for an invasive postmortem.
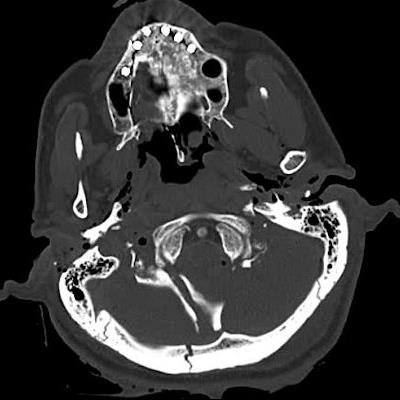
 CT images show catastrophic subarachnoid hemorrhage. All images courtesy of Dr. Lenetta Boyce.
CT images show catastrophic subarachnoid hemorrhage. All images courtesy of Dr. Lenetta Boyce.Kralt is an independent consultant neuroradiologist specializing in forensic radiology and anthropology. He is co-author of the book "Post Mortem CT for Non-Suspicious Adult Deaths: An Introduction." Boyce is a consultant radiologist at Liverpool University Hospitals NHS Foundation Trust, specializing in musculoskeletal radiology and trauma, including stroke.
This discussion was led by radiologists Dr. Uzoma Nnajiuba and Dr. Jamie Howie, the presenters and co-founders of RadCast.
Q: How did you both get into forensic radiology?
Boyce: During the Manchester Arena bombing in 2017, I found out how radiology was involved in that investigation, and then I did some reading and discovered that it was still quite a new topic. When I was training, one of the senior consultants said that you should have a skill that's a little bit different, so I thought forensic radiology would be suitable. It's really interesting -- the more you learn about it, the more you're amazed. I did a postgraduate diploma in it, and my interest developed from there.
Kralt: After completing my radiology training in the Netherlands in 2016, I moved to the U.K. and started to get involved in PMCT. I thought it was a really interesting niche area, and in the past couple of years we've seen a huge increase in numbers. It's an accepted way of investigating death.
Q: What are the indications for PMCT?
Kralt: The vast majority will be non-suspicious deaths in the community. For example, if an elderly person is found deceased by a carer, or a patient who suddenly collapses in the street and subsequently dies, then it's our job to find the cause of death. But you might have a couple of patients whose cases might be slightly more suspicious -- e.g., found at the bottom of the stairs -- and you have to consider whether it was a cardiac event that caused the patient to fall or whether it was something else. Was the patient pushed?
 CT scans performed after a traumatic crush injury. The man was unloading a lorry during a storm when the contents fell on top of him.
CT scans performed after a traumatic crush injury. The man was unloading a lorry during a storm when the contents fell on top of him.Q: Why does someone have a PMCT and not just a traditional postmortem?
Boyce: In the U.K., it often depends on which region you live in. There's a shortage of pathologists, so performing invasive postmortems can be difficult in some parts of the country, so that's where radiology comes in. There may also be religious reasons for PMCTs; in some religions, families are reluctant to wait for a postmortem to be completed to bury their loved one, so offering a PMCT can sometimes help to speed up the process and allow them to put their family member to rest sooner. Also, we'll try to avoid doing an invasive autopsy on children, so again, imaging can help.
Q: Who requests a PMCT?
Boyce: The coroner -- once a person is deceased, the coroner has legal rights over the body. If the medical doctor looking after the patient is unable to give a cause of death, then the case is referred to the coroner, who then decides whether to proceed to an invasive postmortem or a PMCT, depending on what services are available to them in their region.
Q: How is a PMCT performed?
Kralt: We have dedicated protocols for trauma and hanging cases, for example, but the technique is essentially similar to any other CT.
Boyce: Radiation isn't a concern, so you don't have such tight regulations as in clinical practice where you're always trying to dial it down. The bodies are generally scanned in a body bag. Particularly for forensic cases where there's always the chain of evidence to be maintained and the coroner has to document how the evidence (i.e., the body) may have been passed between different areas. Keeping it in the body bag means that the body hasn't been tampered with and there's no contamination of evidence. In some cases, we do a postmortem coronary angiogram and we have to open the body bag to cannulate the vessels to do a CT angiogram.
Q: How do you administer contrast when there's no flowing circulatory system?
Kralt: For a coronary angiography, the embalmer will cannulate the left carotid artery, push the catheter down towards the aortic valve, and then gently flush the contrast into the coronary arteries. That can help to pick up a high-grade stenosis that might have caused an acute myocardial infarct. You can also cannulate the femoral vessels and do a whole-body angiography, even specific arterial and venous series. There's quite a lot of literature on that, but it's not something that we do in normal practice because it's time-consuming and expensive.
 CT image shows type A aortic dissection.
CT image shows type A aortic dissection.Boyce: Some European centres, particularly in Switzerland, prefer a whole-body angiogram, and they use a contrast media injector because it requires about three litres of fluid to opacify the vessels. A group in Leicester, U.K., also uses a CT pump injector for this purpose -- the same as we do for clinical CT. I thought PMCT angiography may be difficult to interpret due to the presence of a lot of clots, but actually, you can often get decent images. Just like in any clinical practice, it's not always perfect. The specialty is still quite new, so no one knows exactly what the best technique is; everyone does it slightly differently. Overall, it's about getting the best images to provide the best diagnosis.
Q: Who decides whether you need to do a postmortem coronary angiography? Is it the coroner or the radiologist?
Kralt: This can vary. We have one facility where the coroner specifically requests an angiogram in virtually all cases, but that's not always necessary. If there's a ruptured aneurysm, there's no need for any coronary angiography because the cause of death is obvious. If the calcium score is significantly elevated, it's difficult to interpret an angiogram and assess the degree of stenosis, similar to an angiogram in the living. But it can be challenging to get that message across to the coroners because they are not all medically trained. You have to try to convince them that more imaging does not always improve the outcome.
Q: How do you report a PMCT if you're not reporting to doctors? Do you have to change your style for a lay audience?
Boyce: We use a template reporting style; there are certain things that you can't comment on, so it makes it easier using a template. We just report what we see, not dissimilar to clinical reporting. You don't mention incidentals because nothing's incidental, is it?
Kralt: You don't have to worry too much about a hyperdense renal cyst, for instance. These are just renal cysts, and they happen to be there and they have no relevance at all once the patient is deceased.
Q: Do you think the stakes are lower because errors are less critical? Are you less worried about missing the minutiae?
Boyce: I think it's the opposite, I don't think there's the worry about missing subtle things, but we are looking for "why did this person die?" We are looking for reasonably obvious pathology. But you do have to be mindful, and you can't be too lackadaisical in what you're reporting because ultimately you could be asked to go to court to provide evidence; you're giving an expert witness statement after all. You have to be mindful that someone could question your report and say, "You said there was no AAA [abdominal aortic aneurysm], but a second opinion has looked and clearly there is a AAA that's ruptured." You answer to the coroner, not the respiratory consultant.
Q: How does the body change on imaging after death? What are the different appearances, and do you have to get used to seeing them? What could be pathology, and what is decay?
 Normal postmortem brain CT with pseudosubarachnoid hemorrhage sign.
Normal postmortem brain CT with pseudosubarachnoid hemorrhage sign.Kralt: Hypostasis is one of the things that we see all the time, which is essentially a normal postmortem finding -- fluid and blood just settling in the dependent areas of the body. So, you always find fluid levels in the aorta and in the superior sagittal sinus; that's all normal.
In the lungs we can find quite extensive ground-glass opacities sometimes, and you may ask: "Well, is this COVID pneumonia?" But this is probably just due to normal fluid that settles in the dependent areas of the lungs, and that's something to bear in mind. If you know the various patterns that may occur, it's fairly easy to understand, but you should also be aware of the fact that normal hypostasis can obscure subtle endobronchial infection.
Boyce: You get used to the patterns of decomposition gas, so seeing portal venous gas is obviously normal in a person that's passed away and sometimes people that haven't been found for a long time have got extensive decomposition; there's a lot of surgical emphysema everywhere. You put the findings that you see up there in the perspective of the clinical situations. For example, a deceased person loses oxygenation of the brain, so the pseudosubarachnoid sign in the brain is a normal postmortem finding. I think the complexity of postmortem imaging is learning what's normal for the deceased.
Q: Is it harder to make a diagnosis, the longer the patient has been deceased? Is there a point where you are unlikely to find the cause of death?
Kralt: Sometimes we scan patients who are severely decomposed, and you can ask yourself the question: the PMCT is not going to help in this case, do we really need to do it? Some coroners insist on scanning all the patients, but if the body is heavily decomposed, it will be very difficult to find a cause of death; it's just gas everywhere there's a pneumothorax, pneumoperitoneum, and then there is decomposition of the soft tissues and even of the bone and then you're not able to find anything apart from maybe aortic and coronary calcifications.
 CT image shows severe decomposition of the abdomen.
CT image shows severe decomposition of the abdomen.Boyce: Ultimately in some of those cases, it's a matter of checking that there's no obvious massive trauma if the skeleton is still intact. Sometimes PMCT can help with identification when the police don't know who that person is. We can try to help the pathologist because they don't have to open up the body bag with a decomposed body inside. We can tell them that the person had a pacemaker or a total hip replacement, which enables them to retrieve the device and look at the serial numbers to possibly trace it back. The person might be wearing jewellery, or sometimes the teeth are still intact so we can try to recreate an orthopantomogram to provide a dental image that can be used to identify the person.
Q: Does reporting PMCTs have a psychological impact on you, especially in paediatric cases?
Boyce: I think you do come across a lot of sad cases, that's the hardest bit for me. You come across these people who have passed away and they haven't been found for weeks and you're thinking, "Gosh, no one thought, no one noticed or recognized, no one knocked on their door."
You come across people that haven't been found because they're widowed. No one's bothered to check on them, and then you see people who have committed suicide.
Editor's note: You can listen to the full podcast and others on the RadCast Anchor page or by searching for RadCast on Spotify, Google, or Apple Podcasts.