Improvements in MRI technique and dynamic imaging -- particularly 3-tesla MRI's ability to demonstrate direct compression of the plexus -- have boosted the diagnosis of neurogenic thoracic outlet syndrome (NTOS), a new Australian study has found.
NTOS is a challenging diagnosis, with delayed diagnosis leading to poorer outcomes, according to Dr. Liam Pugh, a third-year radiology registrar, and Dr. Thomas Lloyd, senior staff specialist in radiology, both at Princess Alexandra Hospital in Woolloongabba, Brisbane, Queensland.
"Imaging the brachial plexus with an MR protocol with dynamic maneuvers can serve as a valuable tool in the diagnostic pathway and surgical planning of patients with clinical features in keeping with NTOS, allowing demonstration of compression of the plexus within the narrowed costoclavicular space," they reported at last week's annual scientific meeting the Royal Australian and New Zealand College of Radiologists (RANZCR), held in Adelaide.
In a poster, they presented a case series involving five patients with positive outcomes following surgical release of such compression.
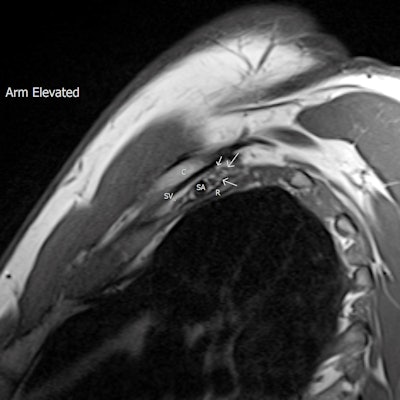
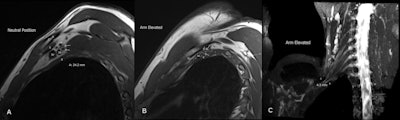 A 34-year-old man with a clinical picture consistent with NTOS. MR images (T1-weighted sagittal) show a capacious costoclavicular space (CS) in the neutral position measuring 24 mm at the narrowest point. With the arm elevated, this reduced markedly to a minimal distance of 4 mm, with the brachial plexus interposed between the clavicle (C) and first rib (R) at this point. Flattening of the subclavian vein (SV) was also demonstrated. No variant anatomy or other cause for compression was seen either radiographically or surgically. (A) Sagittal oblique T1-weighted image at the level of the CS in the neutral position. The CS measures 24 mm in the neutral position, and the divisions of the brachial plexus are clearly outlined by fat (arrows). S = subclavius muscle, SA = subclavian artery. (B) Sagittal oblique T1-weighted image at the level of the CS, arm abducted. The CS is narrowed to 4 mm at the point of the brachial plexus. Arrows = divisions of the brachial plexus. (C) T2 3D SPACE STIR thick MIP reconstruction in coronal plane, level of CS, arm abducted. The CS is narrowed to 4 mm. C5 - T1 nerve roots = labelled. The patient underwent resection of the right first rib with good clinical response. All figures courtesy of Dr. Liam Pugh and Dr. Thomas Lloyd, presented at RANZCR ASM 2022.
A 34-year-old man with a clinical picture consistent with NTOS. MR images (T1-weighted sagittal) show a capacious costoclavicular space (CS) in the neutral position measuring 24 mm at the narrowest point. With the arm elevated, this reduced markedly to a minimal distance of 4 mm, with the brachial plexus interposed between the clavicle (C) and first rib (R) at this point. Flattening of the subclavian vein (SV) was also demonstrated. No variant anatomy or other cause for compression was seen either radiographically or surgically. (A) Sagittal oblique T1-weighted image at the level of the CS in the neutral position. The CS measures 24 mm in the neutral position, and the divisions of the brachial plexus are clearly outlined by fat (arrows). S = subclavius muscle, SA = subclavian artery. (B) Sagittal oblique T1-weighted image at the level of the CS, arm abducted. The CS is narrowed to 4 mm at the point of the brachial plexus. Arrows = divisions of the brachial plexus. (C) T2 3D SPACE STIR thick MIP reconstruction in coronal plane, level of CS, arm abducted. The CS is narrowed to 4 mm. C5 - T1 nerve roots = labelled. The patient underwent resection of the right first rib with good clinical response. All figures courtesy of Dr. Liam Pugh and Dr. Thomas Lloyd, presented at RANZCR ASM 2022.Thoracic outlet syndrome consists of upper limb neurological and vascular symptoms due to compression of the neurovascular bundle as it passes through the thoracic outlet, Pugh and Lloyd explained. Compression may occur within the interscalene space, the costoclavicular space, and the rectopectoralis minor space, but it is most common within the costoclavicular space and is exacerbated by abduction of the arm, which further narrows this space.
The etiology of NTOS is thought to most likely be due to hyperextension neck injury -- which may be minor -- in patients with underlying predisposition due to anatomical variability, they added.
Diagnostic challenges
Vascular thoracic outlet syndrome can be diagnosed with Doppler ultrasound and CT angiography displaying compression/stenosis of the vascular structures. Despite being the more common subtype, with a neurogenic component present in up to 95% of cases of thoracic outlet syndrome, the diagnosis of NTOS is often more challenging, the researchers stated.
"Clinical features are generally vague and overlap with other causes of nerve compression and pain syndromes," they pointed out. "Clinical tests are often positive in asymptomatic volunteers and often rely on arterial compression, which is a poor indicator of neurological compression of the brachial plexus."
The classical presentation is upper limb paresthesia and pain exacerbated by certain shoulder movements including abduction, but the exact location of symptoms varies depending on the level of compression, and weakness and muscle atrophy feature as late signs, according to Pugh and Lloyd.
Neurovascular compressions are often not demonstrated in the neutral position, highlighting the necessity for dynamic MRI. In contrast, the scalene triangle and rectopectoralis minor space demonstrate an equal or lesser degree of compression in thoracic outlet syndrome patients compared to asymptomatic patients.
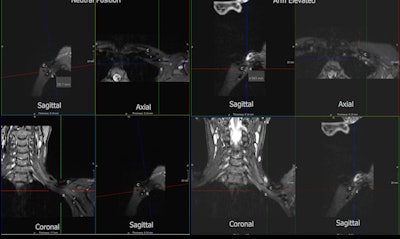 A 49-year-old woman with prolonged symptoms of NTOS, including neck, chest, upper back and upper limb pain, paresthesia, muscle weakness, and muscular atrophy. MRI demonstrated significant narrowing of the costoclavicular space (CS) with the arm elevated narrowing from 26 mm to 5 mm. The patient underwent decompressive surgery with first rib resection and anterior and middle scalenectomy with thoracic outlet syndrome confirmed with the presence of extensive scar tissue surrounding the brachial plexus. Fibromuscular bands between the anterior and middle scalene muscles were also identified. The patient had clinical improvement, but not entire resolution of symptoms, which could relate to the duration of the compression prior to release. (A) T2 3D SPACE STIR 3 planes. Level of CS in neutral position. C = clavicle, R = first rib, A = subclavian artery, V = subclavian vein, CS = measured (26 mm). (B) T2 3D SPACE STIR 3 planes. Level of CS with the arm abducted. The CS is again significantly narrowed to 5 mm.
A 49-year-old woman with prolonged symptoms of NTOS, including neck, chest, upper back and upper limb pain, paresthesia, muscle weakness, and muscular atrophy. MRI demonstrated significant narrowing of the costoclavicular space (CS) with the arm elevated narrowing from 26 mm to 5 mm. The patient underwent decompressive surgery with first rib resection and anterior and middle scalenectomy with thoracic outlet syndrome confirmed with the presence of extensive scar tissue surrounding the brachial plexus. Fibromuscular bands between the anterior and middle scalene muscles were also identified. The patient had clinical improvement, but not entire resolution of symptoms, which could relate to the duration of the compression prior to release. (A) T2 3D SPACE STIR 3 planes. Level of CS in neutral position. C = clavicle, R = first rib, A = subclavian artery, V = subclavian vein, CS = measured (26 mm). (B) T2 3D SPACE STIR 3 planes. Level of CS with the arm abducted. The CS is again significantly narrowed to 5 mm.At the Princess Alexandra Hospital, imaging is performed on a 3-tesla scanner with sequences consisting of 3D SPACE [sampling perfection with application-optimized contrasts using a different flip angle evolution] STIR [short tau inversion recovery] images in a coronal plane orientated to the neurovascular bundle, sagittal Dixon T2 images, and T-weighted images with the imaged volume extending through the supraclavicular fossa to the humerus.
Sequences are performed with the arm in both neutral position and in abduction with external rotation. Additionally, a sagittal T2 cervical spine is performed to assess cervical nerve roots.
Origins of study
Lloyd told AuntMinnieEurope.com that he was initially performing brachial plexus MRI studies for a plastic surgeon in the context of trauma. A vascular surgeon then asked Lloyd if this could be used for NTOS.
"When we worked on the protocol, we realized the need to image in more than one position to assess the interval change in the anatomic spaces, and we had a couple of good clinical outcomes," he remarked.
The project remains a work-in-progress. Lloyd -- who is a network training director at his hospital, a visiting radiologist at BreastScreen Queensland, and an adjunct professor at the Queensland University of Technology (QUT) Faculty of Health -- said he is happy to share the protocol with other sites and radiologists. He hopes this might lead to a larger project.