Ultrahigh-field MRI (UHF-MR) scanners will play an increasingly important role in clinical imaging and cannot be ignored, according to Prof. Thoralf Niendorf, PhD. Ahead of next month's symposium about UHF-MR, he outlines the areas of greatest promise for MRI at 7 tesla and above. He also explains why windsurfing is the ideal cognitive detox.
 Prof. Thoralf Niendorf, PhD.
Prof. Thoralf Niendorf, PhD.Niendorf is professor for experimental ultrahigh-field MRI at the Charité in Berlin and head of the Berlin Ultra High Field facility at Max Delbrück Center for Molecular Medicine. His group's research concentrates on the development of MR methodology and MR technology with a focus on new ways of mapping and probing morphology, function, physiology, and metabolism. The Berlin team also analyzes the benefits and challenges of ultrahigh-field imaging to advance cardiovascular, neurovascular, molecular, and other MRI applications.
This Q&A interview was conducted onsite in Berlin on 23 August 2022.
Q: What's the appeal of conducting human MRI scans at field strengths greater than 7 tesla? Which field strength above 7 tesla makes most sense to you?
A: From a simple radiological view, one of the main motivations is to improve sensitivity or improve the signal-to-noise ratio (SNR) because it scales superlinearly with field strength. This helps to improve the spatial resolution and would allow more detail in the images. But this is a traditional and conventional viewpoint, and we need to consider the economic costs associated with such a development.
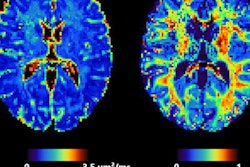
One of the main issues right now is to connect radiology better with biology and physiology. We need to find answers to the question: What is the physiological or biological meaning of the imaging findings? That's why the quest for, or the move to, higher field strengths, including field strengths as high as 14 tesla and 20 tesla, is due to explorations into physiometabolic MRI. This includes sodium imaging, potassium imaging, chloride imaging, imaging high energy phosphates using phosphorus MRI or, for example, imaging inflammatory processes using fluorine MRI.
Moving further down the road involves not just doing functional morphologic imaging but also expanding the clinical MRI portfolio to physiometabolic imaging. And there the sensitivity gain at these higher field strengths is really paying off.
I am very excited that the first 10.5-tesla system is operating at the University of Minnesota in the U.S. The hope is that there are more systems to come. One manufacturer or one vendor has recently announced a 10.5-tesla commercial product, which is very encouraging.
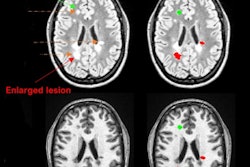
Q: At the annual congress of the International Society for Magnetic Resonance in Medicine (ISMRM) in May, you said that "Imaging lesions is not enough. That would limit us to being photographers. That's why we need to learn more about the mechanisms behind diseases or disorders." Can you elaborate on this point?
A: Our mission is to understand the biological and physiological meaning of the imaging findings. Imaging or counting lesions is not enough because we need to understand the mechanisms behind the lesions. Is a lesion first -- followed by some vascular impairment when we talk about multiple sclerosis lesions -- or does a vascular impairment come first, which is then followed by the lesions? These are very mechanistic questions.
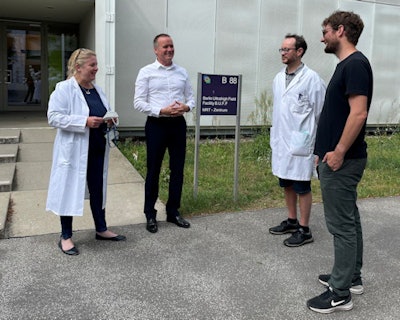 Members of the Berlin team. From left to right are Dr. Sonia Waiczies, principal investigator, experimental ultrahigh-field MR; Thoralf Niendorf; Dr. Jason M. Millward, senior research fellow, experimental ultrahigh-field MR in neuroimmunology; and Ludger Starke, doctoral candidate, experimental ultrahigh-field MR.
Members of the Berlin team. From left to right are Dr. Sonia Waiczies, principal investigator, experimental ultrahigh-field MR; Thoralf Niendorf; Dr. Jason M. Millward, senior research fellow, experimental ultrahigh-field MR in neuroimmunology; and Ludger Starke, doctoral candidate, experimental ultrahigh-field MR.Another field of research, for example, concerns renal MRI. Other than creatinine concentration, there are no clinical diagnostic markers out there to probe acute kidney injury and its progression to chronic kidney disease, and creatinine concentration only shows changes if the injury has already occurred. Our mission, therefore, is to find better diagnostic and prognostic markers at a much earlier stage of the disease progression.
In renal disease, for example, hypoxia is a very key feature of acute kidney injury. Determining whether there is hypoxia is very valuable information, but it's not enough because we want to understand the underlying mechanisms driving the kidney into hypoxia. Connecting radiology or imaging science with physiology and biology is of the utmost importance.
Q: Can you tell us about other exciting future clinical directions of UHF-MR?
A: There are several areas I've got in mind. One area is, again, related to kidney disease and acute kidney injury. There is a major unmet clinical need, and addressing it through renal MRI would significantly improve diagnostic imaging of the kidney as well as improve the development of therapies.
Another area of clinical interest is cardiac UHF-MR. We showed at 7T that prolongation in the myocardial relaxation time T2* is a marker for hypertrophic cardiomyopathy and provides new insights into myocardial microstructure.
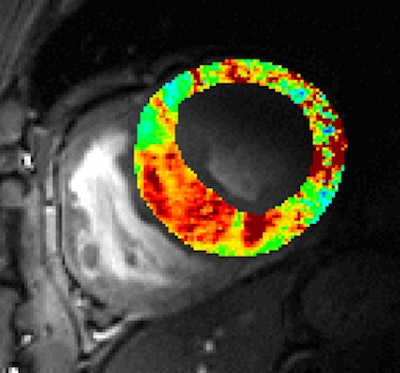 Cardiac T2* map acquired at 7 tesla. The image shows a short axis view of the heart of a patient with hypertrophic cardiomyopathy. Red indicates a prolongation in T2* which is pronounced for myocardial regions with wall thickening. Courtesy of Prof. Thoralf Niendorf.
Cardiac T2* map acquired at 7 tesla. The image shows a short axis view of the heart of a patient with hypertrophic cardiomyopathy. Red indicates a prolongation in T2* which is pronounced for myocardial regions with wall thickening. Courtesy of Prof. Thoralf Niendorf.Right now, the spectrum of therapies is very limited due to the lack of diagnostic markers or tools. If you want to develop a drug or a therapy, you need to have a tool that can be used for monitoring the outcome of the therapy or drug. The goal is not to limit it to these high field strengths but to transfer this technology to lower field strengths. And this can be done: UHF-MR is the steam engine, steaming ahead, but the ultimate goal is to provide tools that are also available at lower field strengths.
Other exciting fields of research are imaging ions, or physiometabolic imaging -- e.g., imaging the sodium content of the skin or of muscle tissue. We have had very nice results demonstrating that the sodium content in the skin changes with age. People can't lie about their age anymore, because we just need to acquire a sodium MRI scan, and based on this, we can determine their biological age, within a certain range.
This has major clinical implications because according to textbook knowledge, there's an equilibrium between sodium intake and sodium output. All these dietary measures and ideas about the salt diet are based on this, but our data show that sodium is deposited in the skin and muscle tissue. These are major deposits of sodium chloride.
All this basically questions conventional knowledge as a foundation of the salt diet, which can help against the risk of hypertension or lowering the blood pressure. This is a major change in paradigm. I could set up an MRI scanner that is being used for sodium imaging 24/7, based upon the research proposals and projects and clinical questions, which can be addressed with sodium MRI.
Q: What role does UHF-MR have to play in imaging of long COVID?
A: Long COVID raises several questions, some of which are related: Is there any change in the micromorphology or morphology of the brain? Is there any impact on cardiac function? And what's the impact on lung tissue?
MRI does not do the best job at imaging the lungs; other imaging modalities are better. But we've been thinking about two avenues of research. One is using ultrashort-echo-time MRI techniques to image the lungs. The other is to use fluorinated samples or compounds to track the signal. Because there's no fluorine in the body, any flaw in the signal that is seen in MRI will be due to the external samples or compounds being used, so it's very much conceivable to use fluorinated gases for inhalation and then to do a fluorine MRI to probe pulmonary function.
Q: You mention in your bio that "ultrahigh-field MRI has earned the moniker of being among the most challenging MRI applications." What makes UHF-MR so challenging?
A: Most of these challenges are related to physics, because the radiofrequency (RF) wavelength in tissue is much shorter than at lower field strengths. In fact, the wavelength is about 13 cm in tissue, so it's much smaller than the size or the geometry of the body or of the target anatomy. This phenomenon induces constructive and destructive interferences in the RF waves in tissue or in the body, which manifests itself as a nonhomogeneity in the image quality or in the signal intensity. This hampers the image quality, which is the main currency in diagnostic imaging. The main challenge is to address these nonuniformities in signal intensity across the images to make the life of radiologists much easier.
Q: There has been much discussion recently about magnetic resonance fingerprinting. What is it, and why is it important?
A: We are not doing any research into MR fingerprinting here, but I recognize this is a hot topic.
The reason why it's so exciting is that it is about quantitative imaging; it's not about just acquiring a series of images that are weighted with a specific MR contrast. It's about mapping specific MR relaxation parameters or any other metrics, and that makes it easier to compare data obtained across different vendors and at different field strengths. This also connects MRI much closer with physiology and biology.
What's the basic principle? As a term, fingerprinting is a bit of a simplification, if not an oversimplification. But if you want to summarize it in a single sentence, it's about tissue characterization, using a series or set of MR metrics that can be acquired in a single scan. Using the conventional approach, you needed to do one scan for getting a T1 map, another scan for getting a T2 map, and so on. With fingerprinting, you are just using the power of the fundamental Bloch equations to acquire a series of images; compare these images with a library, and the outcome will be a set of quantitative maps -- including the T1, T2, etc., relaxation times which can be acquired in a single scan.
Q: Looking ahead to the 13th scientific symposium about UHF-MR on 9 September. What's new this year? How many attendees do you expect? Which topics do you think are most of interest to radiologists? Can you highlight one or two clinical sessions that our readers must not miss?
A: This year's symposium is a hybrid one with some online and some in-person participation. That, one might say, is a silver lining of the pandemic. With this approach, we are now able to reach out to a larger audience and cover a broader spectrum of time zones.
We expect about 350 to 450 attendees. There will be a presentation on the design of the world's first 14-tesla human MRI system, and the speaker will demonstrate that such an instrument is feasible. That addresses many concerns and questions that have been roadblocks in the past, but at least this talk is going to demonstrate the technical feasibility. The good news is this talk has been provided by one of our collaborators, an entrepreneurial team based in Magdeburg, Germany.
We also want to provide a glimpse into the future. For example, we have made some explorations into making a diagnostic imaging device into an interventional device by integrating some changes into the MRI scanner. For this purpose, we are using RF-induced heating to heat up targeted areas in the tissue as a kind of adjunct therapy to chemotherapy and radiotherapy. This is a very interesting topic because RF-induced heating or RF power deposition is being considered a faux.
There are legal limits for the amount of RF power deposition in the tissue induced by a diagnostic MRI examination. Every MR scanner has a limit that is laid down by the International Electrotechnical Commission (IEC) guidelines. If the RF power deposition exceeds this limit, the scanner will shut off automatically to protect the tissue from heating. With our technology however, we can deliberately target tissue with any arbitrary shape and geometry. This also makes the imaging device an interventional device and adds a new dimension to MRI.
I am keen to inform the radiology community about this feature. Of course, it's going to take a bit more time to turn it into a commercial product, but I'm quite sure everyone will want to learn about what's going to happen in the next three to five years.
 A thrilling hobby like windsurfing that requires intense concentration can help to prevent burnout, says Niendorf.
A thrilling hobby like windsurfing that requires intense concentration can help to prevent burnout, says Niendorf.Q: Outside of MRI, you've told us before about your love for windsurfing. Did you go on any special trips over the summer?
Niendorf: Yes, I went to the Baltic Sea in the northern part of Germany, and we had the best winds ever for windsurfing. I was out during a perfect storm, which lasted for three days. It was three days of flying above the water -- we call this planing -- while being in the foot straps. It is not as easy as it might look like on YouTube because it requires a flawless synchronization between the brain and several tiny muscles down to your toes to keep the magic triangle between the board, the sail, and the body and to fly in the right direction. Any distraction of the brain will throw you right away from the board into the water. Planing is the best cognitive detox!