Radiologists from the John Radcliffe Hospital in Oxford, U.K., have found there is room for improvement in reducing radiation dose during barium swallow studies. They've recommended taking a fresh look at training in this area.
"The findings from the present study are in support of revisiting consultant-supervised [barium swallow studies] training, which might help lowering the radiation exposure for patients," wrote consultant radiologists Dr. Mitchell Chen and Dr. Horace D'Costa wrote (Clinical Radiology, April 22, 2022).
Barium swallow studies were the first-line investigation at one time for many upper gastrointestinal pathologies. In recent years, the procedure has been mostly superseded by esophagogastroduodenoscopy (EGD) procedures. However, barium swallow studies retain important roles in the investigation of dysphagia, epigastric pain, and persistent vomiting because of its less invasive nature over EGD.
A key drawback of barium swallow studies is its exposure of patients to ionizing radiation. The radiation dose of barium swallow is thought to be operator-dependent and can be reduced through staff training, the authors noted.
Thus, in this investigation, the researchers aimed to elucidate the issue by exploring the relationship between the operator's level of training and radiation dose in barium swallow studies at their hospital.
The investigators first compared radiation doses used in 1,004 barium swallow studies against the U.K.'s current recommended national diagnostic reference level (NDRL), which is 750 cGy*cm2, down from a level of 1,200 cGy*cm2 in 1995. The tests were performed using an Artis Zee multipurpose angiography system (Siemens Healthineers) at John Radcliffe Hospital between December 2016 and June 2018.
Next, Chen and D'Costa looked at radiation doses used in the studies with operators stratified by training levels. The operators were categorized as radiology trainees, advanced radiography practitioners, GI radiology fellows, and GI radiology consultants.
Most of the cases (68.2%) reported radiation doses compliant with the NDRL. However, there was a statistically significant difference between operators based on their levels of training, with the observed mean dose decreasing with advancing training status of the operator, the researchers found.
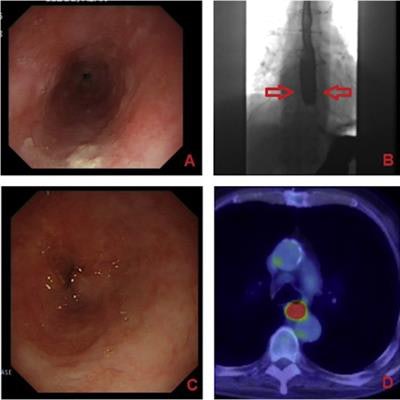
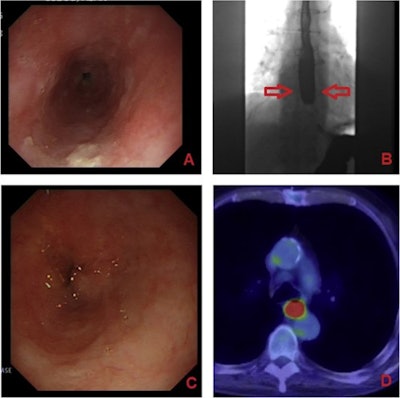 Barium swallow studies in practice: A 71-year-old male first presented with retrosternal pain and dysphagia. The initial esophagogastroduodenoscopy (A) had a histological diagnosis of tubular adenoma. The barium swallow showed mild dysmotility and hold-up in the distal esophagus (B, pointed to by the red arrows). A normal-appearing esophagus was shown on CT three months later, but a repeat EGD was performed six months later due to progressive dysphagia, which showed "suspicious appearing fibrotic stenosis in mid-distal esophagus" (C) with squamous cell carcinoma demonstrated on histology. This was then confirmed on F-18 FDG PET/CT staging as an FDG avid carcinoma in the mid-distal esophagus (D). Image courtesy of Clinical Radiology.
Barium swallow studies in practice: A 71-year-old male first presented with retrosternal pain and dysphagia. The initial esophagogastroduodenoscopy (A) had a histological diagnosis of tubular adenoma. The barium swallow showed mild dysmotility and hold-up in the distal esophagus (B, pointed to by the red arrows). A normal-appearing esophagus was shown on CT three months later, but a repeat EGD was performed six months later due to progressive dysphagia, which showed "suspicious appearing fibrotic stenosis in mid-distal esophagus" (C) with squamous cell carcinoma demonstrated on histology. This was then confirmed on F-18 FDG PET/CT staging as an FDG avid carcinoma in the mid-distal esophagus (D). Image courtesy of Clinical Radiology.Boxplot sample data points showed large numbers of test doses above 1,200 cGy*cm2 for advanced practitioners and radiology trainees, while mean doses for consultants and fellows were below 500 cGy*cm2, according to the findings.
"The fact radiation dose was found to be related to operator's level of training, with the lowest doses reported for those performed by GI radiology consultants, support the study hypothesis and that further radiation dose reduction can be achieved through operator training by senior GI radiologists," the authors stated.
Increasing evidence supports the idea of radiographers assuming an expanded role in diagnostic fluoroscopic investigations, with comparable diagnostic accuracy reported for barium swallows performed by the trained radiographers and those by radiologists. This move is favored, since it frees up GI radiology consultants from having to acquire the images so they can instead focus on checking and reporting on the acquired images, the authors wrote.
However, the issue of radiation dose reduction should not be overlooked in this matter, the authors suggested.
"Overall, expanding the role of GI radiology consultants in the training of junior radiologists and advanced radiography practitioners is needed," Chen and D'Costa concluded.