MRI is an effective modality for assessing osteoarthritis (OA) and bone marrow edema, according to Prof. Dr. Siegfried Trattnig of the Medical University of Vienna. He offered a primer on this topic at the recent Arab Health 2022 meeting in Dubai.
 Prof. Dr. Siegfried Trattnig at Arab Health 2022. Image courtesy of Robert Stevens.
Prof. Dr. Siegfried Trattnig at Arab Health 2022. Image courtesy of Robert Stevens.Osteoarthritis causes changes in the biochemical composition of cartilage, which consists of collagen and proteoglycans, he noted. Collagen is the framework of cartilage, and proteoglycans, which include glycosaminoglycans (GAGs), are part of its extracellular network. A decrease in GAGs and increased water content in the cartilage are early signs of degeneration.
How can these biochemical changes be identified? MRI offers a number of techniques that produce "compositional" images of the cartilage, stated Trattnig.
"[These MRI] techniques attempt to selectively demonstrate the GAG components and/or the collagen fiber network of the extracellular matrix and are usually summarized as 'compositional imaging' of cartilage," he said. "These MR methods have recently gained increasing importance as imaging biomarkers used as primary endpoints in the monitoring of the efficacy of surgical cartilage repair procedures as well as in clinical trials with newly developed cartilage anabolic drugs."
Trattnig outlined four MRI techniques for imaging osteoarthritis:
- Delayed gadolinium enhanced MRI of cartilage (dGEMRIC). "dGEMRIC is based on the fact that GAGs contain negatively charged [amino acid] side chains, which lead to an inverse distribution of negatively charged contrast agent molecules (that is, gadolinium) with respect to GAG concentration," he said. This technique does have drawbacks, including the need for a double dose of gadolinium-based contrast and a delay between contrast administration and the MRI exam.
- T2 and T2* mapping. Studies have shown that T2 mapping can assess the composition of articular cartilage in the knee by defining collagen structure and water content, and researchers have explored the use of T2* mapping for imaging collagen as well, according to Trattnig. "Cartilage T2 values seem to be associated with the severity of osteoarthritis," he said.
- Sodium imaging. The benefit of this technique for musculoskeletal applications is that it is "specific to glycosaminoglycan content and, since the sodium from surrounding structures in the joint is low ... articular cartilage can be visualized with very high contrast without the requirement for any exogenous contrast agent such as that in dGEMRIC," Trattnig noted. The emergence of 7-tesla whole-body MRI scanners has made sodium imaging more feasible. Drawbacks? It requires special hardware and radiofrequency coils.
- Texture analysis -- Gray-level co-occurrence matrix (GLCM). This technique improves T2 mapping by producing data on cartilage features such as homogeneity or entropy, Trattnig noted. "With careful parameter and feature selection we can probe the underlying structural information from the T2 maps of cartilage and the changes caused by osteoarthritis or maturation of repair tissue," he said.
| Characteristics of MRI techniques for visualizing early osteoarthritis | ||||
| Type of technique | Cartilage component | Contrast? | Exam time | Spatial resolution |
| dGEMRIC | GAG-specific | Yes | 10 minutes | 0.6 x 0.6 mm |
| T2 mapping | Collagen network and water content specific | No | 6 minutes | 0.6 x 0.6 mm |
| Sodium MRI | Highly GAG-specific | No | 20 minutes | 1.5 x 1.5 mm (on 7-tesla) |
| Texture analysis of GLCM | Additional information | No | 0 minutes | Enhanced T2 mapping |
MRI for bone marrow edema
Bone marrow edema is often diagnosed using MRI and has a variety of causes that fall under two general categories, Trattnig noted: reactive (rheumatoid disease, osteoarthritis, tumor, inflammation, fractures, and bone bruises) and ischemic (osteonecrosis, bone marrow edema syndrome, osteochondritis dissecans). It is also categorized as traumatic or nontraumatic.
"Traumatic bone marrow edema is common after direct or indirect trauma, is usually found [in the epiphyseal plate], and mirrors trauma biomechanics," he said.
MRI can identify the following bone marrow pathologies, according to Trattnig:
- Bone marrow edema syndrome. Manifests as sudden knee or hip pain without trauma.
- Transient migratory idiopathic bone marrow edema syndrome. Manifests as a "diffuse bone marrow edema pattern with complete resolution," although it may "fluctuate for years," he noted.
- Spontaneous insufficiency fracture. Often seen in elderly women with acute pain not prompted by trauma; manifests in an "ill-defined bone marrow edema pattern," according to Trattnig.
- Spontaneous osteonecrosis of the knee. This condition is a fracture in bone underneath cartilage without evidence of bone tissue death, he noted.
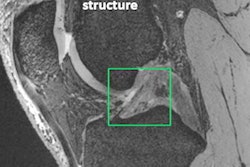
- Bone marrow edema in osteoarthritis. This condition has a structure comparable to stress fractures and no bone tissue necrosis, Trattnig said. But osteoarthritis pain is strongly associated with bone marrow edema, and the combination of osteoarthritis and bone marrow edema increases the likelihood of total knee replacement ninefold.
"With MRI, bone marrow edema-related entities such as bone marrow edema syndrome can be differentiated from femoral head necrosis, subchondral insufficiency fractures, and spontaneous osteonecrosis of the knee -- which is important since therapy will be different," Trattnig told AuntMinnieEurope.com.