Researchers have proposed a three-step approach to the diagnosis of appendicitis in pregnant women based on accurate appendix localization and assessment of primary and secondary signs of appendicitis using MRI, as well as keeping in mind alternative pathologies for exclusion.
"With the increasing utilization of emergency MRI and the relatively high incidence of abdominal pain in pregnancy, interpretation of acute abdominal pathology in an obstetric patient on MRI is becoming an increasingly relevant skill for the radiologist covering a tertiary center's out-of-hours call -- and one which can make a significant clinical impact," noted Dr. Arjuna Somasundaram, a radiologist at Queensland X-Ray and Gold Coast University Hospital, Australia, and his colleague Dr. Cassandra Jeavons.
Acute appendicitis is the primary reason for nonobstetric surgical intervention during pregnancy, and it has an estimated incidence of 1/1,500 pregnancies, they explained in an e-poster presentation at the recent Royal Australian & New Zealand College of Radiology (RANZCR) annual scientific meeting.
"Appendicitis can be a challenging clinical diagnosis in pregnancy due to multiple confounding factors; cecal displacement and abdominal distension from the gravid uterus, as well as pregnancy-related physiological leucocytosis can all confuse the clinical picture," they wrote.
A delayed diagnosis of appendicitis significantly increases morbidity and mortality to both the fetus and mother. Overdiagnosis is also problematic, as negative laparotomy rates in obstetric patients with suspected appendicitis is around 25%-50% without MRI, exposing patients to an unnecessary risk of early labor and increased fetal mortality. Early diagnosis may also help to triage certain patients into a trial of conservative management with antibiotics or toward surgery.
The authors gave the following advice on how best to diagnose appendicitis in pregnancy with MRI.
Step 1: Localize the appendix
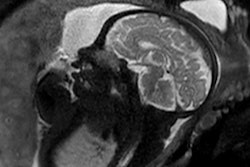
As with CT, localizing the appendix can be a difficult task, given its wide variation in position. The cecal tilt angle can be assessed on sagittal T2-weighted MRI -- an angle of at least 90° localizes the appendix to the right upper quadrant with high specificity irrespective of gestational age, they pointed out.
Subsequent localization of the appendix may require concurrent use of multiple planes. The T2 nonfat saturated half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence often provides sufficient spatial resolution to identify the appendix, while T2 fat-saturated HASTE can help localize the region of interest through its high sensitivity for fluid and oedema. In difficult cases, the gradient-echo sequence may assist by emphasizing appendiceal intraluminal gas or calcifications through the blooming artifact.
Step 2: Identify primary and secondary signs of acute appendiceal inflammation
An obstructing appendicolith, appendiceal diameter larger than 6 mm (outer wall to outer wall), and T2 wall hyperintensity are all suggestive of acute appendicitis. Without other primary or secondary findings, an appendix diameter larger than 6 mm alone has demonstrated less sensitivity than the other aforementioned primary findings of acute appendicitis, the authors wrote.
Secondary features include T2 hyperintense edema of the mesoappendix or surrounding mesentery, intraperitoneal free fluid, and para-appendiceal or paracecal phlegmonous mass. The presence of secondary appendiceal signs without primary signs should raise suspicion for a diagnosis of early appendicitis in the absence of any alternate abdominal pathology.
Step 3: Review for other common causes of acute abdominal pain
Hemorrhagic fibroid degeneration is commonly associated with pregnancy and can be identified as a T1 hyperintense rim around a fibroid. The ovaries should be specifically reviewed to evaluate for ovarian cyst rupture and ovarian torsion, according to the researchers. A large field-of-view T2 sequence can be used to localize acute inflammation of the kidney or gallbladder, and similarly, obstructing renal calculi, hydronephrosis, or small bowel obstruction can be identified.
MRI protocol in Queensland
Ultrasound is the primary test in the investigation of acute abdominal pain in pregnancy, but its sensitivity is highly dependent on the end user's experience. Ultrasound's sensitivity for the diagnosis or exclusion of appendicitis in pregnancy has been reported as low as 46%, pointed out Somasundaram, who also works as a lecturer at Griffith University, South-East Queensland, having completed a fellowship in cross-sectional imaging in Toronto, Canada, in 2019.
In contrast, MRI for acute appendicitis in pregnancy is very accurate, and a systematic review of 19 studies found an overall sensitivity and specificity of 91.8% and 97.9% respectively, he reported.
At Queensland X-Ray, MRI tends to be reserved for cases in which ultrasound and clinical findings are inconclusive. The team's protocol for acute appendicitis in pregnancy consists of axial, coronal, and sagittal T2-weighted HASTE (for anatomical detail); axial and coronal T2-weighted fat-saturated HASTE (higher sensitivity for edema and fluid); and axial T1-weighted gradient echo sequences in and out of phase (identification of blood products or appendiceal gas/appendicolith).
1.5 or 3-tesla MRI can be used, but 1.5T is generally preferred due to the reduction in motion artifact, the authors continued. Intravenous gadolinium is contraindicated due to the potential risk of fetal gadolinium transfer, and oral contrast is not used.
"Despite the theoretical risks to the fetus associated with MRI in the first trimester, we generally do not restrict MRI in this group for two reasons: one, the evidence linking first trimester MRI with poor fetal outcomes is relatively weak, with guidelines varying between major organizations; and two, the risks associated with a delayed diagnosis of appendicitis are likely to be much higher than that from MRI-related effects," they stated.
Editor's note: You can view the authors' clinical images by going to the link to the full poster on the RANZCR section of the Electronic Presentation Online System (EPOS) on the European Society of Radiology's website.