Why are international guidelines so important in everyday clinical practice, and how do patients benefit from them? Prof. Dr. Mike P. Wattjes from the Institute for Diagnostic and Interventional Neuroradiology at Hannover Medical School is the lead author of new international recommendations on multiple sclerosis (MS) imaging. He discusses the new guidance in a Q&A interview with the German Röntgen Society (Deutsche Röntgengesellschaft, DRG).
Q: MS is a chronic inflammatory disease of the central nervous system. Around 250,000 people are affected in Germany. What role do radiology and MRI play in the diagnosis and treatment of MS?
 Prof. Dr. Mike P. Wattjes. Photo courtesy of Karin Kaiser, Hannover Medical School (MHH).
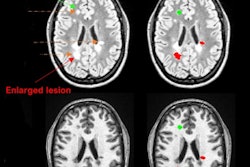
Prof. Dr. Mike P. Wattjes. Photo courtesy of Karin Kaiser, Hannover Medical School (MHH).A: MRI in MS has grown in importance in recent years. It used to be the case that the older diagnostic criteria were based on almost purely clinical and laboratory findings. With improvements in MRI and its wider availability, it has virtually revolutionized diagnosis and the monitoring of disease progression: Due MRI's sensitivity, we can show changes in the brain and spinal cord without the patient showing clinical symptoms. This enables MS to be diagnosed at an early stage, i.e., at first neurological attack.
Furthermore, this is particularly important for monitoring progress because you do not want to see any more disease activity during therapy. MRI provides the neurologist with indications, for example, of whether the patient's medication is efficient enough or whether the treatment needs to be intensified or switched to an even more effective treatment.
Q: Together with experts from various countries, you have now developed new international guidelines for MS imaging in routine clinical practice. How important is it that doctors work according to uniform standards internationally when dealing with this disease?
A: It is very important that this standardization of MS imaging has an international footing because essential questions that we have to answer now and in the future for MS patients depend on large datasets, namely datasets that are standardized and thus comparable, i.e., they allow essential prediction models with regard to individual disease progression.
Prediction models can only be developed with huge datasets. As far as the future use of automated image evaluation algorithms is concerned, we are also dependent on large, standardized datasets. These are only possible if there is a medical agreement on a certain basic standard -- nationally and internationally.
Q: Are you a pioneer in developing the guidelines for multiple sclerosis or have you refined existing ones?
A: These 2021 guidelines are based on further development of guidelines that were already presented by different groups in 2015 and 2016. These guidelines are of course constantly in flux, as there are always new developments in MS, new drugs coming onto the market, and controversial discussion about the use of gadolinium-based contrast media, etc.
In this respect, there have been several developments that have prompted us to revise and refresh the existing guidelines. In addition, it was very important to us to homogenize these different guidelines from Europe and North America into one large global guideline.
Q: How long did the process of developing the mission statement take you and the group of experts you worked with?
A: I always said to my wife that it took two pregnancies, so 18 months. It was a very busy and exciting time, and by the end of this process, we were all a bit exhausted. At the end of the day, the only thing that will help you through this exhausting and time-consuming process is knowing your responsibility to the patient. Guidelines are important -- not primarily for us personally, but primarily for the patient, for medical development by the pharmaceutical industry, and for neurologists and (neuro) radiologists.
Q: What recommendations do you and your colleagues give in the new guidelines, for example on the subject of contrast agent administration?
A: This topic was one of our main motivations for revising existing guidelines. In 2015, we recommended using contrast-enhanced T1-weighted sequences in order to document inflammatory disease activities and thus also to investigate whether a drug therapy is efficient or not. But we have now taken recent discussion about the deposition of elemental gadolinium in the deep gray matter as an opportunity to revise this aspect.
We are now of the opinion that for many questions, especially with regard to therapy monitoring, contrast media are no longer absolutely necessary. There are good alternative markers for active T2 lesions, i.e., with new demyelinating foci, or foci of discoloration that are 50% larger compared with the reference examination.
Of course, there are still indications where contrast media are useful, such as for diagnosing MS. However, for many indications that relate to progress monitoring, therapy efficiency monitoring, and safety monitoring, contrast media are no longer absolutely necessary.
Q: Critics sometimes complain that guidelines, even if they are evidence-based, can be of inadequate methodological quality. They see in this the danger that the recommendations contained in the guidelines will not achieve the desired effect of better patient care if they are implemented. What do you think of this criticism?
A: This criticism is partly justified. Often, guidelines cannot be based exclusively on evidence because there is not enough class 1 evidence to be able to base them on. Many aspects of guidelines, including our recommendations, are often based on many years of experience in routine clinical practice. This is somewhat controversial.
Personally, I do not see criticism of existing guidelines as negative because the moment there is criticism of guidelines, a dialogue also arises. I experience or interpret a critical dialogue as fruitful, to improve things even further. In principle, guidelines are not the gold standard but are intended to guide medical professionals and support them in making the right decisions in routine clinical practice. But they are not mandatory. There are clinical situations in which one can justifiably disregard a guideline.
Q: In which medical specialties do you currently see a particular benefit or a particular need for guidelines?
A: These are topics or specialist areas for which the available data are often inconclusive and very difficult to interpret. This applies both to radiological and diagnostic topics as well as to the therapy of certain diseases. A good example is the current and recently published German Neurology Society (Deutsche Gesellschaft für Neurologie, DGN) guideline for MS.
The MS therapy landscape is becoming ever broader and more heterogeneous, and here too it is important to offer doctors orientation and assistance in order to pave the way for the best possible therapy decision for the benefit of the individual patient.
Editor's note: This is an edited version of a translation of an article published in German online by the DRG on 23 June 2021. Translation by Frances Rylands-Monk. To read the original version, go to the DRG website.