FDG-PET/MRI combined with ultrasound could reduce the need for invasive biopsy to confirm suspicious findings in women with newly diagnosed metastatic breast cancer, according to a study by German researchers published on 20 May in the Journal of Nuclear Medicine.
The study found that FDG-PET/MRI outperformed sonography, breast MRI, and thoracic MRI for the detection of axillary lymph node metastases, as well as that FDG-PET/MRI when combined with ultrasound may achieve a level of accuracy that could obviate the need for invasive biopsies.
"If both imaging modalities show a positive nodal status, it could be taken into consideration to even dispense axillary histopathological sampling," wrote first author Dr. Janna Morawitz of the University Dusseldorf in Germany.
Studies indicate up to 40% of early breast cancer patients show axillary nodal metastatic disease at the time of diagnosis, which suggests axillary intervention represents overtreatment for about 60% of patients. Breast MRI, sonography, and CT have become well established for the initial staging of breast cancer patients.
Yet, so far, no imaging modality has proven to be accurate enough to replace invasive biopsy procedures for determining the correct nodal status, according to the authors.
In this prospective, multicenter study, the researchers conducted a head-to-head analysis of hybrid FDG-PET/MRI imaging and sonography, breast MRI, and thoracic MRI for the detection of axillary lymph node metastases in 112 women with newly diagnosed, therapy-naive breast cancer. Patients (mean age, 53.04 ± 12.6 years) were diagnosed between March 2018 and December 2019.
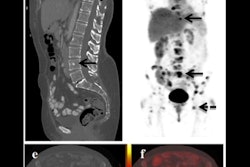
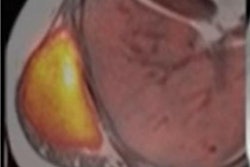
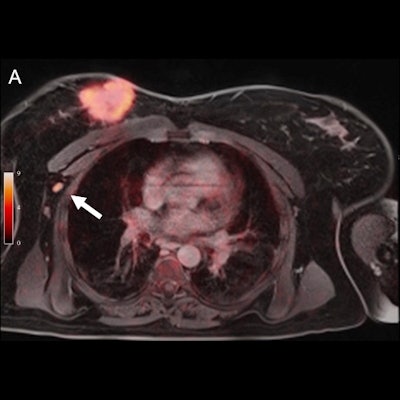
 Pathologically confirmed axillary lymph node metastasis that was correctly identified on F-18 FDG PET/MRI (A) because of tracer uptake above background levels (SUVmax 4.3) and in axillary sonography (B) because of cortical enlargement to 3.8 mm (short-axis diameter 8 mm). This lymph node was rated unsuspicious on thoracic MRI (C) and breast MRI (C). Large primary cancer is seen in the right breast (D). Figure courtesy of Journal of Nuclear Medicine.
Pathologically confirmed axillary lymph node metastasis that was correctly identified on F-18 FDG PET/MRI (A) because of tracer uptake above background levels (SUVmax 4.3) and in axillary sonography (B) because of cortical enlargement to 3.8 mm (short-axis diameter 8 mm). This lymph node was rated unsuspicious on thoracic MRI (C) and breast MRI (C). Large primary cancer is seen in the right breast (D). Figure courtesy of Journal of Nuclear Medicine.Histopathology served as a reference standard in every patient, while area under the receiver operating characteristic curve (AUC) values were used to measure performance. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated for all four modalities.
Thoracic PET/MRI showed the highest ROC-AUC with a value of 0.892. The AUC for breast MRI was 0.782; thoracal MRI was 0.814; and sonography was 0.834. Differences between the modalities were statistically significant. PET/MRI also showed the highest sensitivity (81.8%, 36/44), while axillary sonography had the highest specificity (98.5%, 65/66).
| Performance of imaging modalities for detecting metastatic breast cancer | ||||
| Sonography | Thoracic MRI | Breast MRI | Thoracic PET/MR | |
| Sensitivity | 69.1% | 63.6% | 61.4% | 81.8% |
| Specificity | 98.5% | 97.1% | 95.6% | 95.6% |
| Positive predictive value | 96.7% | 93.3% | 90.0% | 92.3% |
| Negative predictive value | 83.3% | 80.5% | 79.3% | 89.0% |
| Accuracy | 87.04% | 83.3% | 82.1% | 90.2% |
"In our study, [F-18] FDG PET/MRI demonstrated the best diagnostic performance in detecting nodal positive patients compared to the other modalities," the researchers stated.
Given that ultrasound had the highest specificity, the authors suggested future workflows should consider performing FDG-PET/MRI as a "searching tool" before clip-marking of the primary tumor, if applicable in clinical workflow, and then adding axillary sonography to specify findings.
The authors added that although tissue pathology remains the final determiner of the N-stage, knowledge of the higher sensitivity of PET/MRI compared with the other modalities will help in the growing field of targeted biopsy in the future.
"Further prospective studies would be needed to investigate the potential replaceability of sampling by this approach," they concluded.