FDG-PET/CT is the modality of choice for staging and assessing cancer patients, but whole-body MRI can make a valuable contribution to detection and diagnoses where the hybrid modality underperforms, ECR 2021 registrants learned at a special session on Sunday evening.
Given its lack of radiation and no need for a radiotracer, MRI can be a highly effective imaging option for the detection of metastatic disease in almost all organs, including prostate cancer, and its array of imaging sequences can discover lesions and nodes unseen by FDG-PET/CT in cases of lymphoma.
"Whole-body MRI, as the name indicates, is an all-organ screening method," said Dr. Frédéric Lecouvet, PhD, professor of radiology at the Université Catholique de Louvain in Brussels. "We will detect not only bone metastases but also with T1-weighted sequences we can see lymph node metastases and with diffusion-weighted MRI we will see bone and node metastases in one single examination."
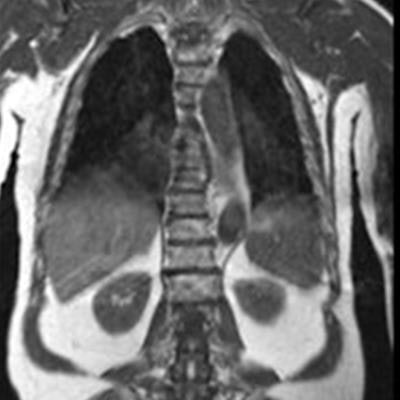
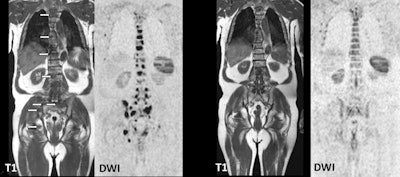 Images show a prostate cancer patient's evolution from multifocal skeletal metastases to normal marrow appearance. Coronal T1- and diffusion-weighted imaging (DWI)-MRI (two left images) show multiple foci of low signal intensity corresponding to metastases (arrows). After systemic therapy, follow-up images (right two images) show complete disappearance of the lesions and return to normal homogeneous signal intensity of the bone marrow. Images courtesy of Dr. Frédéric Lecouvet, PhD.
Images show a prostate cancer patient's evolution from multifocal skeletal metastases to normal marrow appearance. Coronal T1- and diffusion-weighted imaging (DWI)-MRI (two left images) show multiple foci of low signal intensity corresponding to metastases (arrows). After systemic therapy, follow-up images (right two images) show complete disappearance of the lesions and return to normal homogeneous signal intensity of the bone marrow. Images courtesy of Dr. Frédéric Lecouvet, PhD.FDG-PET/CT has long set the imaging benchmark for the diagnosis and treatment response assessment to a multitude of cancers, given its "reliable quantification, is almost free of artifacts, and is established in many clinical guidelines," added Dr. Marius Mayerhöfer, PhD, an associate professor of radiology at the Medical University of Vienna. "It is not widely available, though, which is one advantage for MRI, which is widely available and does not use ionizing radiation. In terms of functional information, [MRI] is somewhat limited, it is not standardized, and it is prone to artifacts."
So how then might whole-body MRI be of value to cancer patients? In prostate cancer cases, MR images rival prostate-specific membrane antigen (PSMA)-PET/CT, which currently is considered the best nuclear medicine imaging modality for this specific application, Lecouvet said. By comparison, whole-body MRI performs just as well for bone metastatic disease, but PET is better at the detection of small lymph nodes.
"It all begins with newly diagnosed disease in patients at high-risk for metastases," he told ECR 2021's virtual attendees. "We have to distinguish those [patients] with no metastases who may benefit from a local radical treatment from those with high-volume metastases who will benefit from systematic treatment."
Whole-body MRI, for example, allows for the detection of early metastatic disease, known as oligometastasis, for which specific metastasis-targeted treatments appear highly promising to improve patient outcome, Lecouvet added. The modality also aids in the monitoring of advanced metastatic disease where several treatment options remain available. In addition, MRI has transposed successfully to other cancers providing metastases to bone, as well as to almost all organs, and is used in breast or neuroendocrine cancers, melanomas, liposarcomas, and -- last but not least -- in hematologic cancers, such as multiple myeloma.
In fact, Lecouvet advocated that both whole-body MRI and PSMA-PET/CT replace bone scintigraphy and CT for the optimal detection of metastatic disease during new diagnoses and recurrence of prostate cancer, adding that MRI has shown its superiority to bone scintigraphy in the detection of bone metastases for almost three decades.
Given the pros and cons of both modalities, FDG-PET/CT and whole-body MRI could play parallel roles to benefit lymphoma patients, especially since both modalities have their drawbacks.
There are a number of different lymphoma subtypes -- including the most common, Hodgkin lymphoma -- which are consistently FDG-avid and fairly easy to characterize through PET/CT. On the other hand, other forms of the disease, such as marginal cell lymphoma, chronic lymphocytic leukemia (CLL), and small lymphocytic lymphoma (SLL) are FDG-avid in only approximately half of the cases, which is a "clear limitation," Mayerhöfer said. "That is why in the current Lugano classification [for lymphoma staging], some lymphomas should not undergo FDG-PET/CT for workup ... and others should go to contrast CT."
Might MRI then be used where FDG-PET/CT for lymphoma underperforms? One problem is that there currently are no recommendations for whole-body MRI in the clinical guidelines for this application.
"That is a bit unfortunate and also a bit unfair," added Mayerhöfer, who also serves as director of PET/MRI at Memorial Sloan Kettering Cancer Center in New York City. "MRI performs quite well in lymphomas, especially when you use diffusion-weighted imaging (DWI), and because lymphoma types with a rather high cell density allow clinicians to indirectly quantify cellularity [through MRI]."
He offered ECR 2021 virtual attendees several examples of SLLs and CLLs in which lymphadenopathy showed very little uptake of FDG and abnormalities were almost impossible to see on CT. DWI-MRI, however, "beautifully" showed evidence of lesions in the liver and in the stomach. "Therefore, the histological subtitle of lymphoma is of high relevance for imaging," Mayerhöfer said. "In those lymphomas, which should not undergo PET/CT, according to the guidelines, DWI-MRI was better than all techniques including contrast-enhanced CT."
DWI-MRI is not a panacea for all lymphoma imaging. When scanning the head and neck, the MRI sequence might not correctly classify malignant inflammatory nodes. Motion artifacts also are a "major concern, especially in the neck area, which is an important anatomic region for lymphoma, where we could find disease," he said. "That is one of the reasons why whole-body MRI is not as popular as FDG-PET/CT at the moment."
On the other hand, previous studies have shown that whole-body MRI can perform very well with aggressive lymphomas. "Altogether [MRI] is good, but not quite as good as FDG-PET/CT, as we found in our study of different lymphoma subtypes," Mayerhöfer said. "We saw that it is really the lymph nodes that are a problem. The sensitivity of MRI for nodal disease is not quite as good as FDG-PET/CT, whereas for extranodal disease, [MRI's] performance is almost perfect, almost on par with PET."
As for the future of whole-body MRI in oncology, the radiology community "has to focus on the reduction of artifacts, standardization of apparent diffusion coefficient (ADC) calculations, so we can better use it for treatment response assessment and perhaps for patient outcome and prognosis," he concluded.