FDG-PET scans and cognitive function tests showed that patients with chronic COVID-19 who suffer from neurological impairment had not yet returned to normal after six months in a recent study by German researchers.
The authors used FDG-PET scans to measure neocortical glucose metabolism and the Montreal Cognitive Assessment (MoCA) test to measure cognitive function in COVID-19 patients once they were no longer infectious (subacute stage) and six months after the onset of symptoms (chronic stage). In comparison with a control cohort, both measures improved, but patients exhibited residual hypometabolism and average MoCA performance rates still within the range of mild cognitive impairment.
"Although a significant recovery of regional neuronal function and cognition can be clearly stated, residuals are still measurable in some patients six months after manifestation of COVID-19," said Dr. Jonas Hosp and colleagues at the University of Freiburg, Germany.
Cognitive impairment is a frequent complaint in COVID-19 patients. Impaired memory, disturbed concentration, and cognitive problems have been reported two to four months after the onset of symptoms and have been related to cortical hypometabolism on F-18 FDG PET at the subacute stage. However, it is unclear if these changes are reversible.
In this prospective analysis published online on 31 March in the Journal of Nuclear Medicine, researchers investigated whether cognitive impairment and the hypometabolism in the cortex were reversible after six months after COVID-19 resolved.
The group enrolled patients with confirmed SARS-CoV-2 infection who had at least one novel neurological symptom developed under COVID-19 and required inpatient treatment at the University Hospital Freiburg between 20 April 2020, and 10 June 2020. A total of 31 subacute COVID-19 patients were assessed for impaired cognitive functions with the MoCA test.
Seventeen of these patients had undergone an F-18 FDG-PET examination. Of those, eight patients underwent a second examination with F-18 FDG-PET and MoCA testing at the chronic stage of the disease and were included in this study. Eight patients refused further investigations because they had no more self-perceived complaints. One patient died.
Group analysis using statistical parametric mapping revealed a widespread increase of F-18 FDG uptake in frontoparietal and, to a lesser extent, temporal neocortical regions in patients in the chronic stage compared to the subacute stage. No regions with significant decrease in glucose metabolism were identified. Voxel-wise comparison of chronic-stage patients to the age-matched control cohort confirmed the presence of a remaining neocortical hypometabolism in COVID-19 patients even at the chronic stage at an exploratory statistical threshold.
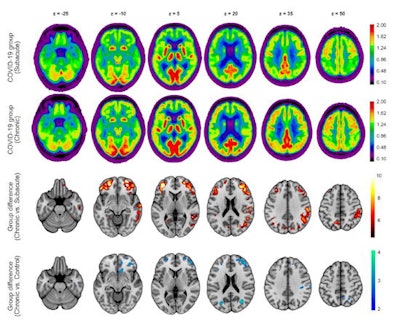 Results of the F18-FDG PET group analysis. First and second row: Transaxial sections of group averaged, spatially normalized F-18 FDG PET scans in patients at the subacute and chronic stages. Third and fourth rows: Regions that show significant increases of normalized F-18 FDG uptake in patients at the chronic compared with the subacute stage. Fourth row: Regions that still show significant decreases of normalized F-18 FDG uptake in patients at the chronic stage compared with the age-matched control cohort (two-sample t test, p < 0.005). Statistical parametric mapping t-values are color coded and overlaid onto an MRI template. Images are presented in neurologic orientation: the left image side corresponds to patients' left body side; numbers denote axial (Z) position in mm. Image courtesy of the Journal of Nuclear Medicine.
Results of the F18-FDG PET group analysis. First and second row: Transaxial sections of group averaged, spatially normalized F-18 FDG PET scans in patients at the subacute and chronic stages. Third and fourth rows: Regions that show significant increases of normalized F-18 FDG uptake in patients at the chronic compared with the subacute stage. Fourth row: Regions that still show significant decreases of normalized F-18 FDG uptake in patients at the chronic stage compared with the age-matched control cohort (two-sample t test, p < 0.005). Statistical parametric mapping t-values are color coded and overlaid onto an MRI template. Images are presented in neurologic orientation: the left image side corresponds to patients' left body side; numbers denote axial (Z) position in mm. Image courtesy of the Journal of Nuclear Medicine.Performance on the MoCA test significantly improved over time, from a mean global score of 19.1 ± 4.5 (maximum 30 points) at the subacute stage to 23.4 ± 3.6 at the chronic stage; however, the scores were still below the frequently used cutoff value for detection of cognitive impairment (< 26/30), according to the authors. Five of eight patients were still below this threshold. MoCA scores showed that orientation and attention were almost unimpaired at the chronic stage, but they revealed persistent deficits in visuoconstructive and executive functions and, especially, memory.
Ultimately, the researchers noted they demonstrated essential reversibility of decreased neocortical glucose metabolism assessed by F-18 FDG PET scans accompanied by an improvement of cognitive functions in COVID-19 patients from the subacute to the chronic stage after a SARS-CoV-2 infection.
However, in comparison to a control cohort, chronic COVID-19 patients still exhibited a slightly higher pattern of expression (at trend-level) and residual hypometabolism, which indicates a shift toward normal levels, but not a definite return, they said.
"Given the current pandemic situation and tremendous uncertainty concerning the long-term effects of COVID-19, the present study provides novel insights of highest medical and socioeconomic relevance," the authors concluded.