Both 3D volume rendering (VR) and maximum intensity projection (MIP) are clinically useful imaging modalities for visualizing complex liver anatomy, but 3D VR provides additional features absent from MIP, according to research posted in the European Journal of Radiology.
In a study involving hepatic malignancies, 3D VR outperformed MIP in its ability to isolate individual structures with color enhancement and calculate the volume of defined regions of interest. Image rotation and small vessel clarity was adequate with both modalities, noted first author Dr. Joyce L. Ho, from the City of Hope Comprehensive Cancer Center, Duarte, California, and Riverside Community Hospital, Riverside, California, and colleagues.
"3D volume rendering has broad applications in the identification of imaging biomarkers such as perfusion, textural analysis, and density variations Integration of artificial intelligence with advance imaging can increase its efficiency," they noted in an article posted by the EJR on 5 September. "While MIP is also useful for quickly generated images, the additional features of 3D imaging such as color enhancement and volumetric analysis make it more widely applicable for precise anatomic reconstruction.
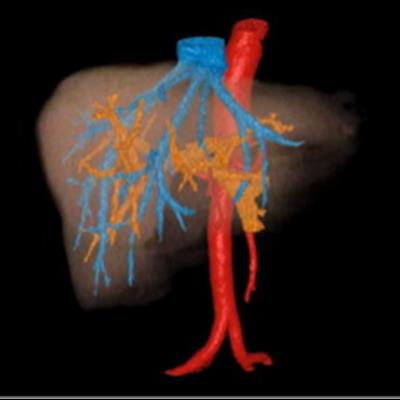
 Color-enhanced 3D volume-rendered (VR) images of the liver in a patient with hepatic malignancy (left), with isolation of vascular structures (right). Red = hepatic arteries arising from the aorta; blue = hepatic veins leading to the inferior vena cava; orange = portal venous system; brown = liver parenchyma. All images courtesy of the EJR and Dr. Joyce L. Ho.
Color-enhanced 3D volume-rendered (VR) images of the liver in a patient with hepatic malignancy (left), with isolation of vascular structures (right). Red = hepatic arteries arising from the aorta; blue = hepatic veins leading to the inferior vena cava; orange = portal venous system; brown = liver parenchyma. All images courtesy of the EJR and Dr. Joyce L. Ho.The quality of images generated by both modalities is influenced by contrast quality and software capabilities, which should be optimized for high quality images, and new developments in the field of advanced 3D imaging can have profound clinical implications on surgical planning and tumor mapping.
Hepatic vascularity
The team assessed the utility of 3D VR and MIP for anatomic delineation of hepatic vascularity. Contrast-enhanced abdominal CT images from patients with malignancies involving the liver who were undergoing surgical evaluation at the City of Hope Helford Hospital between 2009 and 2015 were initially reviewed by experienced academic radiologists.
All initial images had been obtained as part of routine care. Of the studies from 128 patients, only 38 were done with multiphase protocols including both arterial and venous phases. Images were reconstructed into 0.625 x 1.25-mm slices for postprocessing and uploaded to General Electric Advanced Workstation Server 3.2 for analysis. 3D MIP images were generated by merging arterial and venous phase images with a "drag and drop" tool.
2D images were registered using nonrigid automatic registration. Studies with limited MIP clarity due to motion artifact and suboptimal contrast enhancement were excluded from further analysis. The Volume Computer Assisted Reading (VCAR) software was used to generate scaled 3D images of the 13 studies that had suitable MIP images.
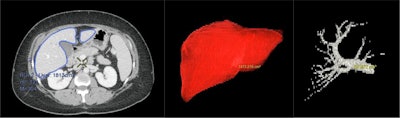 Volume calculation on 3D VR images. The liver is defined as the region of interest (left), and the Volume Computer Assisted Reading (VCAR) software extrapolates the defined region to additional CT slices. The VR Compare application can then calculate the volume of the entire liver (center) or an individual structure, such as the portal vein (right).
Volume calculation on 3D VR images. The liver is defined as the region of interest (left), and the Volume Computer Assisted Reading (VCAR) software extrapolates the defined region to additional CT slices. The VR Compare application can then calculate the volume of the entire liver (center) or an individual structure, such as the portal vein (right).3D color-enhanced volume rendering was performed using the CT arterial and venous phase images. The images were imported in to GE AW workstation, and quantitative volumetric assessment was performed using the automatic hepatic VCAR tool with manual edits when needed. The hepatic artery, hepatic vein, and portal vein were extracted manually based on Hounsfield unit thresholds and were colored individually. Liver lobes were segmented using the virtual scalpel, and color enhancement was applied.
Overall, color enhancement could only be applied with 3D VR imaging and not MIP imaging. Volume calculation and isolation of liver segments were also possible with 3D VR but not MIP imaging. Image rotation in the superior to inferior, the anterior to posterior, and the lateral view was achieved with both modalities. Vessel delineation was better visualized with 3D VR imaging. The clarity of individual small vessels was suitable with both modalities. The overall performance indicates that 3D VR is the superior methodology to delineate the anatomical features, compared with the MIP.
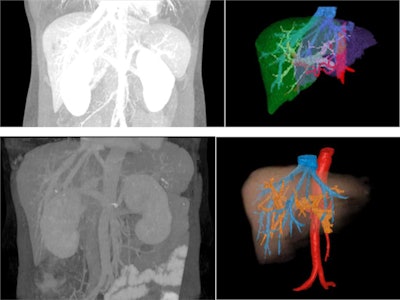 Comparison MIP and 3D VR images from two patients with hepatic malignancy. The borders of the overlapping portal and hepatic vessels are the same intensity in the monochromatic MIP images, but smaller vessels can be clearly visualized. The overlapping hepatic and portal veins and their branches can be delineated on the color-enhanced 3D VR images.
Comparison MIP and 3D VR images from two patients with hepatic malignancy. The borders of the overlapping portal and hepatic vessels are the same intensity in the monochromatic MIP images, but smaller vessels can be clearly visualized. The overlapping hepatic and portal veins and their branches can be delineated on the color-enhanced 3D VR images."Imaging is an essential component of the preoperative evaluation," the authors wrote. "MRI has high soft-tissue resolution and can detect hepatic lesions without radiation exposure. However, it is limited by slow scanning speed, and motion artifact."
2D CT and MRI used to detect hepatic tumors underrepresent 25%-30% of cases, while 3D or perfusion imaging techniques may provide additional information with increased accuracy in the clinical setting, they added.
What are the pros and cons?
MIP creates a 3D perspective by projecting images onto a viewing plane, while preserving attenuation information. The technique is useful in visualizing simple anatomic structures, but it lacks the ability to depict spatial depth and differentiate superimposed structures. On arterial phase-dominant images, venous structures can appear more posterior than they actually are in relation to arterial structures. MIP is limited by motion artifact from vessel pulsation and respiration, which also rendered many of our initial images for this study inadequate.
"3D volume rendering is a useful technique for tumor staging and surgical mapping. As this study illustrates, individual structures can be highlighted and quantified on 3D volume rendered images," the authors noted. "However, 3D VR requires manual editing individual CT slices to ensure accurate isolation of the region or structure of interest. This time-consuming task can be a barrier to routine utilization. Automating this process is an evolving area of research that make 3D imaging more efficient and readily available."
The application of quantitative 3D color mapping can increase the sensitivity and diagnostic performance of CT. Recent studies suggest quantitative perfusion analysis also increases the sensitivity and specificity of CT for detection and anatomic delineation of hepatocellular carcinoma. There is no added radiation exposure with postprocessing 3D VR, and its application can offer greater anatomic visualization at the cost of the computer software, Ho and colleagues concluded.



















