Extending telework to nonmedical areas of the radiology department during the COVID-19 crisis can significantly help protect staff and patients, while ensuring productivity and associated cost savings, according to Spanish researchers.
A team predominantly from HT Médica, a group of outpatient centers in Andalucia and La Mancha, describe in a new paper how teleworking during the COVID-19 pandemic has highlighted its value beyond radiological interpretation -- with the current situation providing opportunities for reorganizing workflow and developing new projects.
"The summer has been of 'tense calm' with regard to our organization and in general for the Spanish healthcare system," HT Médica's medical director, Dr. Antonio Luna Alcala told AuntMinnieEurope.com. "Although, the number of COVID-19 cases in Spain has been the highest in Europe, the pressure on the health system and HT Médica has been under control."
He noted that physical meetings had been reduced to the minimum, replaced instead by online work.
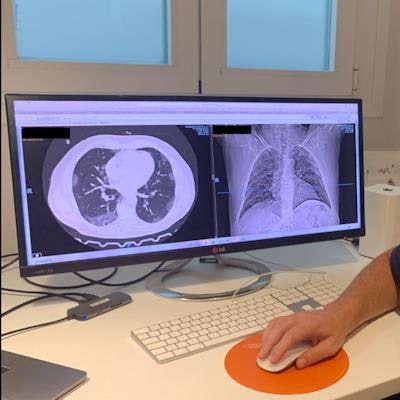
 Dr. Antonio Luna Alcala teleworking from home. All images courtesy of Drs. Antonio Luna Alcala and Teodoro Martín Noguerol et al.
Dr. Antonio Luna Alcala teleworking from home. All images courtesy of Drs. Antonio Luna Alcala and Teodoro Martín Noguerol et al.His colleague Dr. Teodoro Martín Noguerol, head of neuroradiology, pointed to a new increase in the number of COVID-19 cases, which could be indicative of a second wave of novel coronavirus infections. But he also noted that the group's imaging department is prepared.
"Teleradiology and teleworking ratios have increased in our institution not only to maintain the quality of our studies and administrative tasks but specifically as part of the protective measures for radiologists," Martín Noguerol said.
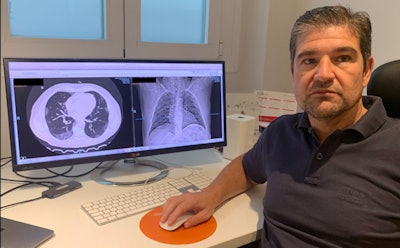
 Telework protocols are helping imaging staff smoothly adjust to the second wave, according radiologist Dr. Teodoro Martín Noguerol.
Telework protocols are helping imaging staff smoothly adjust to the second wave, according radiologist Dr. Teodoro Martín Noguerol.While imaging workload decreased by 80% during the peak of the pandemic, thanks to telework adjustments, HT Médica worked at almost full capacity for noncare tasks, avoiding any positive COVID-19 cases in the radiology department.
"Now, we have normal care workload and we are able to manage it with approximately 50% of our radiologists working from home, and almost 100% of nonmedical tasks (administration, human resources, IT, billing) performed through telework. Indeed, lessons learned from the first wave are allowing us to adjust to this second wave without any extra effort," he said.
The group is currently evaluating the degree of satisfaction of both workers and managers, trying to define the role of teleworking in the organization while also establishing clear policies for the optimal IT infrastructure that the workforce needs to work from home.
In their paper, "Teleworking beyond teleradiology: managing radiology departments during the COVID-19 outbreak," published in European Radiology on 2 September, the authors noted that the use of teleradiology and teleworking solutions in the new paradigm imposed by COVID-19 is helping imaging departments to combat infection while maintaining productivity and cost savings.
However, the authors sounded caution:
"Transition of all operative areas to a full teleworking experience is not easy and needs a strong IT infrastructure, including remote connection to the electronic health record (EHR) or hospital information system (HIS). There is also a need to provide access to Admission, Discharge, and Transfer (ADT) systems, and billing and auditing systems to maintain the basic functions of the department, particularly processes linked to patient throughput, safety, and experience," they noted.


Direct communication is key to creating solid networks between all the personnel involved in telework in order to minimize disinformation or isolation, as well as allowing a flexible schedule for those teleworking, which will optimize their effectiveness.
The authors advocated the use of web-based scheduling solutions to minimize the risk of potential new infections. Such solutions play an important role in preparing safe worklists and minimizing patient time in the department -- the latter through the completion of all related administrative tasks during the online scheduling process. Such scheduling tools can also be used to increase the time slots between radiological exams to facilitate proper equipment cleaning between patients, the authors noted.
New opportunities
Another silver lining to the situation is that radiologists may have more time to invest in education and research, due to changes in workflow and workload, according to the authors. This might entail helping research groups to develop and move projects forward, improving and updating protocols, and performing internal audits.
They also pointed to other opportunities such as online continuous training of fellows or residents, completing unfinished scientific manuscripts, and development of artificial intelligence algorithms for COVID-19 and for other clinical radiological purposes, adding that teleconference platforms, shared calendars, and worksheets reflecting project status including deadlines would help team organization.
HT Médica runs the radiology departments of six private hospitals, and it has been using teleradiology since the mid-1990s to increase its radiologists' degree of specialization, as well as to optimize their worklists. While it has more than 50 onsite radiologists, all HT Médica centers function via teleradiology and work as a single department particularly for emergency room readings.
"With the advent of the outbreak, we established parallel teams of radiologists, many of them working from home, to keep only the minimum workforce necessary in the centers," Alcala said. "Because the organization has a high degree of digitalization and decentralization, administrative and support departments are located in different cities, and centers and are used to working online with digital tools."
By the end of February, the group imposed teleworking for all nonmedical workers. Computers, laptops, and printers were relocated from offices to homes and the IT department established virtual private networks with the EHR and HIS.
"Without any doubt, teleworking will [continue to] play a major role in our organization once the outbreak is finished," noted Alcala.



















