The emergence of 3D printing, along with volume rendering and 3D modeling software, is making it easier to define complex cardiovascular anatomy and extracardiac vascular structures, and these technologies now play a pivotal role in the diagnosis of congenital heart disease (CHD), award-winning Spanish researchers have reported.
"Radiologists should be familiar with key imaging findings and with the advantages and limitations of these techniques in order to establish an optimal therapeutic approach and management," noted radiologist Dr. Flavio Zuccarino and colleagues from the Hospital del Mar and Hospital Sant Joan de Déu in Barcelona, Spain.
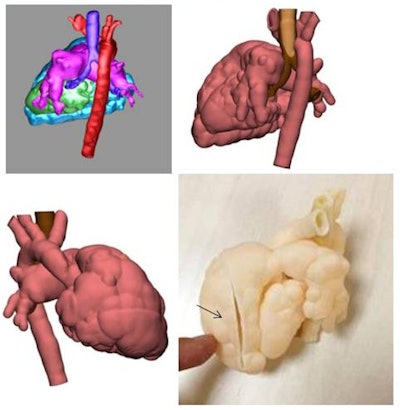 3D printed model of pulmonary valve agenesis in a newborn obtained from a 3D model created with CT images. Note the complex cardiovascular anatomy and relationship between vessel and airways. The surgeon can observe the interior ventricular cavity by means of a cut made in the ventricle surface (arrow) and can then decide on the most suitable surgical treatment or pulmonary prosthesis. All images courtesy of Hospital Sant Joan de Déu, Barcelona.
3D printed model of pulmonary valve agenesis in a newborn obtained from a 3D model created with CT images. Note the complex cardiovascular anatomy and relationship between vessel and airways. The surgeon can observe the interior ventricular cavity by means of a cut made in the ventricle surface (arrow) and can then decide on the most suitable surgical treatment or pulmonary prosthesis. All images courtesy of Hospital Sant Joan de Déu, Barcelona.Echocardiography represents the first imaging tool in the diagnosis of CHD, but extracardiac structures can be difficult or impossible to detect, and cardiovascular CT is becoming increasingly important, they explained in an ECR 2020 e-poster presentation that received a certificate of merit.
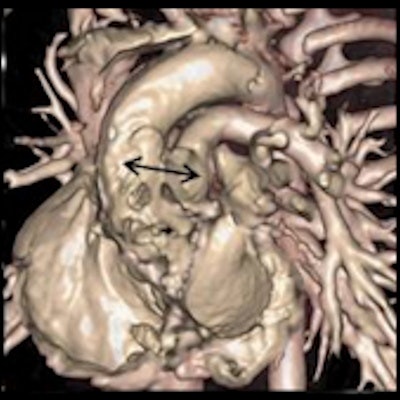
Coarctation of the aorta represents a congenital narrowing of the aortic arch. CT can assess associated CHD, and this is valuable in the management of these patients. "CT represents the best noninvasive technique for the evaluation of coarctation treated with intravascular stents, and can even depict postsurgical complications," Zuccarino and colleagues pointed out.
Interrupted aortic arch is a rare form of coarctation characterized by the lack of luminal continuity between ascending and descending aorta. CT can define the level of aortic obstruction and the presence of the patent ductus arteriosus (PDA), a persistent opening between the two major blood vessels leading from the heart.
Aortopulmonary window (AP window) is a rare anomaly that represents a communication between the main pulmonary artery and the ascending aorta. CT can evaluate the presence of both aortic and pulmonary valves as well as the location and size of the AP window, and it can differentiate the AP window from truncus arteriosus.
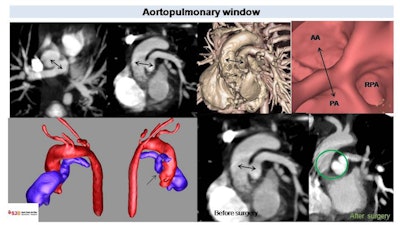 CT in 2-year-old patient with Tetralogy of Fallot. Note the communication between the main pulmonary artery (PA) and ascending aorta (AA) (black arrows) corresponding to the aortopulmonary window. Volume rendered and endoscopic images show vessel distribution at this level. Postsurgical image depicts absence of communication between the aortic and pulmonary lumen (green circle). RPA = right pulmonary artery.
CT in 2-year-old patient with Tetralogy of Fallot. Note the communication between the main pulmonary artery (PA) and ascending aorta (AA) (black arrows) corresponding to the aortopulmonary window. Volume rendered and endoscopic images show vessel distribution at this level. Postsurgical image depicts absence of communication between the aortic and pulmonary lumen (green circle). RPA = right pulmonary artery."3D models help in the evaluation of vessel anatomy and in the presurgical planning," the authors explained.
Awareness of the following additional main points is essential, they stated:
- Pulmonary artery stenosis, observed in different CHD cases, may be key in planning surgical treatment. CT can evaluate the course of pulmonary arteries or stenosis treated with intravascular stents.
- Pulmonary atresia is characterized by an atretic pulmonary valve and different degrees of anomalies of pulmonary arteries. CT can define pulmonary arteries' morphology, shape, and size, and it can demonstrate a PDA or the presence of major aortopulmonary collateral arteries (MAPCAs). Absence of the pulmonary is a rare anomaly in which the pulmonary circulation is only supplied by MAPCAs, which are large collateral vessels that connect the systemic circulation to the native pulmonary arteries. CT can assess their course and morphology and their relationship with surrounding structures.
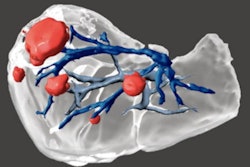
- In complex anomalies of pulmonary veins, such as Scimitar syndrome, CT can identify pulmonary vein connections or associated findings as pulmonary hypoplasia or sequestration. In total anomalous pulmonary venous return, 3D images represent the best technique to define this complex venous anatomy.
- In cases of Tetralogy of Fallot, CT can depict all the anatomic features of patients and may be useful in the analysis of pulmonary artery stenosis or dilation. CT evaluation of associated anomalies such as right aortic arch and anomalous origin of coronary arteries can have an impact on surgical strategy.
- The bicuspid aortic valve (BAV) is the most common source of CHD and may lead to aortic stenosis or regurgitation. When BAV is extremely calcified, CT can be used. CT can evaluate associated aortic arch anomalies.
- CT and 3D images are key to determine correct prosthesis positioning. Volume-rendered images easily depict a correct positioning into pulmonary valve of a self-expanding pulmonary valve. "We can easily define an incorrect position due to early displacement of a self-expanding pulmonary valve on the right, where the prosthetic pulmonary valve is displaced into the right ventricular outflow tract, parallel to pulmonary artery long axis, and its diameter is enlarged," Zuccarino and colleagues wrote.
- The persistent left superior vena cava (PLSVC) usually drains into the right atrium through a dilated coronary sinus. In some patients, PLSVC drains into the left atrium, generating right-to-left cardiac shunt. CT easily defines the presence of PLSVC as its drainage and is key in the management of these patients. When PLSVC is accompanied by a normal right-side vena cava, a double superior vena cava exists, where right vena cava drains into the right atrium.
"This work has been realized because in Hospital Sant Joan de Déu we have a 3D center dedicated to pediatric 3D models," Zuccarino told AuntMinnieEurope.com. "Radiologists collaborate with engineers and clinicians to produce models. I'm the person responsible for the cardiovascular radiology. Also, we have a dedicated course about 3D imaging and models, called the Expert 3D course."
Editor's note: To view the authors' full e-poster and clinical images, go to the European Society of Radiology's EPOS website.