Cardiac MRI shows that patients who have recovered from COVID-19 may be at risk of heart complications, according to a study conducted by German researchers and published on 27 July in JAMA Cardiology.
The study findings suggest yet another facet of the illness that must be tracked, wrote a team led by Dr. Valentina Puntmann, PhD, of University Hospital Frankfurt in Germany.
"[In our study], cardiac magnetic resonance imaging revealed cardiac involvement in 78 patients (78%) and ongoing myocardial inflammation in 60 patients (60%)," the group wrote. "These findings indicate the need for ongoing investigation of the long-term cardiovascular consequences of COVID-19."
Thus far, most research on COVID-19 has focused on the disease's respiratory effects, but there has been increasing evidence of cardiovascular effects as well, according to the authors.
"A number of case reports and small series suggested that COVID-19 prominently affects the cardiovascular system by exacerbating heart failure in patients with preexisting cardiac conditions and troponin elevation in critically ill patients," they wrote. "[But] there remains poor insight into the cardiovascular sequelae in unselected patients, including those with no preexisting conditions, who were not hospitalized, or had no or only mild symptoms."
Puntmann and colleagues conducted a study that included 100 patients identified through the University Hospital Frankfurt COVID-19 Registry who had recovered from COVID-19 disease between April and June. All patients underwent cardiac MRI; median time between COVID-19 diagnosis and cardiac MRI was 71 days. The group matched recovered patients by sex and age to control groups of healthy volunteers (50) and risk-factor matched patients (57). Of the 100 recovered patients, 67% recovered at home and 33% were hospitalized.
The investigators found the following:
- 78% of patients had abnormal findings on cardiac MRI, including raised myocardial native T1 (73%), raised myocardial native T2 (60%), myocardial late gadolinium enhancement (32%), and pericardial enhancement (22%).
- 71% of patients had high-sensitivity troponin T (which can indicate heart muscle damage); this was significantly elevated (13.9 pg/mL or greater) in 5% of patients. High-sensitivity troponin T correlated with native T1-weighted and T2-weighted mapping.
- Compared to the control groups, recovered COVID-19 patients had lower left ventricular ejection fraction, higher left ventricle volumes, and higher left ventricle mass.
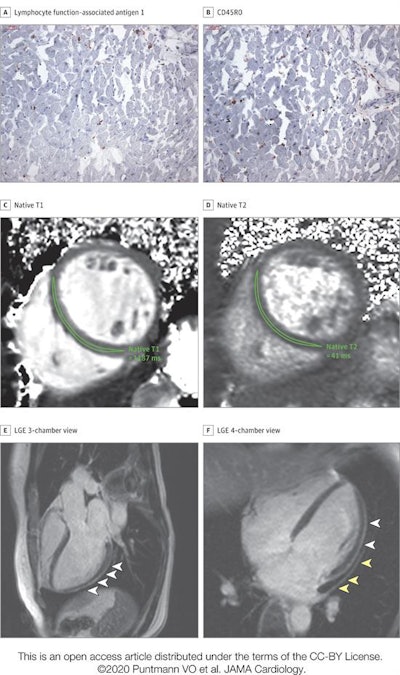 High-sensitivity troponin T level on the day of cardiac MRI was 17.8 pg/mL. The patient recovered at home from COVID-19 illness with minimal symptoms, which included loss of smell and taste and only mildly increased temperature lasting two days. There were no known previous conditions or regular medication use. Histology revealed intracellular edema as enlarged cardiomyocytes with no evidence of interstitial or replacement fibrosis. (A and B) Immunohistochemical staining revealed acute lymphocytic infiltration (lymphocyte function-associated antigen 1 and activated lymphocyte T antigen CD45R0), as well as activated intercellular adhesion molecule 1. (C and D) Cardiac MRI revealed enlarged volumes in myocardial mapping acquisitions, including significantly raised native T1 and native T2. (E and F) Pericardial effusion and enhancement (yellow arrowheads) and epicardial and intramyocardial enhancement (white arrowheads) were seen on late gadolinium enhancement (LGE) acquisition. Images and caption courtesy of JAMA Cardiology.
High-sensitivity troponin T level on the day of cardiac MRI was 17.8 pg/mL. The patient recovered at home from COVID-19 illness with minimal symptoms, which included loss of smell and taste and only mildly increased temperature lasting two days. There were no known previous conditions or regular medication use. Histology revealed intracellular edema as enlarged cardiomyocytes with no evidence of interstitial or replacement fibrosis. (A and B) Immunohistochemical staining revealed acute lymphocytic infiltration (lymphocyte function-associated antigen 1 and activated lymphocyte T antigen CD45R0), as well as activated intercellular adhesion molecule 1. (C and D) Cardiac MRI revealed enlarged volumes in myocardial mapping acquisitions, including significantly raised native T1 and native T2. (E and F) Pericardial effusion and enhancement (yellow arrowheads) and epicardial and intramyocardial enhancement (white arrowheads) were seen on late gadolinium enhancement (LGE) acquisition. Images and caption courtesy of JAMA Cardiology."The most prevalent abnormality [on cardiac MRI] was myocardial inflammation (defined as abnormal native T1 and T2 measures), detected in 60 patients recently recovered from COVID-19 ... followed by regional scar and pericardial enhancement," the group noted.
The study results paint a grim picture, according to an accompanying editorial written by Dr. Clyde Yancy of Northwestern University in Chicago and Dr. Gregg Fonarow of the University of California, Los Angeles.
"We are inclined to raise a new and very evident concern that cardiomyopathy and heart failure related to COVID-19 may potentially evolve as the natural history as this infection becomes clearer," Yancy and Fonarow wrote. "The concerns [raised here] are not theoretical but instead practical and require our due diligence to study and prepare for what may be another dimension of the COVID-19 crisis."