FDG-PET has again proved its value by correlating positive neuroendocrine tumors in patients treated with peptide receptor radionuclide therapy (PRRT) to their chances of overall and progression-free survival, according to a study published on 13 March in the Journal of Nuclear Medicine.
FDG-PET/CT also complimented results from gallium-68 (Ga-68) somatostatin receptor (SSTR) PET/CT after treatment with PRRT, in which high levels of SSTR expression combined with negative FDG uptake to predict more favorable longer-term outcomes.
"Although not generally used for the diagnosis of neuroendocrine tumors, FDG-PET/CT was able to classify neuroendocrine tumor patients into different prognostic categories for PRRT," wrote the authors, led by Dr. Jingjing Zhang, PhD, from Zentralklinik Bad Berka in Germany. "A very high [standardized uptake value] on FDG-PET would at least lead to reconsider the decision to perform PRRT as the first-line procedure."
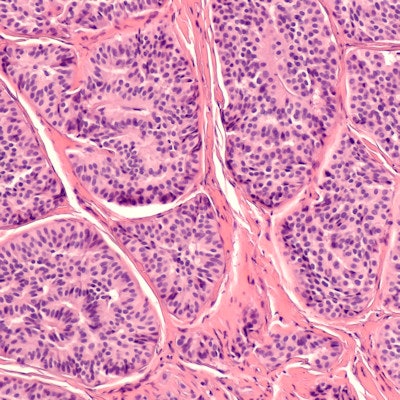
PRRT is considered an especially effective treatment for patients with neuroendocrine tumors because it binds to cancer-related somatostatin receptors on neuroendocrine tumor cells, while healthy cells remain unharmed. With the growing importance of PRRT in treating neuroendocrine tumors, the "relevant outcome predictors are becoming increasingly significant to optimize the application of PRRT," Zhang and colleagues wrote.
To determine which factors predict positive patient response, the researchers retrospectively analyzed data from 495 patients (median age at first treatment, 59 ± 10.7 years; range, 19-80 years) between February 2002 and July 2018 who had metastatic neuroendocrine tumors and high SSTR expression. The subjects underwent both FDG-PET/CT and Ga-68-SSTR PET/CT before receiving treatment with lutetium-177 (Lu-177) and/or yttrium (Y-90)-DOTATOC/DOTATATE PRRT therapy.
The researchers then followed the patients with CT, MRI, or PET before each PRRT cycle, at restaging every three to four months after PRRT, and every six months for stable disease or remission after initial follow-up until disease progression.
FDG-PET/CT showed positive uptake for tumors among 382 patients (77%), while 113 cases (23%) were negative before PRRT. Those initial findings played statistically significant roles in determining a patient's progression-free survival and overall survival, with FDG-avid patients eventually having shorter overall and progression-free survival. Conversely, an FDG-negative result represented a 5% decrease in the risk of death and a 7% decrease in the risk of disease progression.
| Survival of neuroendocrine tumor patients based on FDG-PET results | |||
| Positive FDG results | Negative FDG results | p-value | |
| Progression-free survival | 18.5 months | 24.1 months | 0.0015 |
| Overall survival | 53.2 months | 83.1 months | < 0.001 |
As for Ga-68-SSTR uptake in the primary tumor, the results helped predict overall and progression-free survival, but Ga-68 SSTR-PET was not as proficient as FDG-PET, and the researchers found no direct correlation between maximum standard uptake value Ga-68 SSTR-PET and overall survival. For example, patients with a level 2 liver tumor burden in Ga-68-SSTR PET had a statistically significant lower risk of progression (hazard ratio [HR], 0.5; p = 0.001), but there was no statistically significant decrease in risk in patients with level 3 burden (HR: 0.9; p = 0.664) or level 4 (HR: 0.9; p = 0.256).
Given the results, Zhang and colleagues concluded that clinicians should think twice about the need to perform PRRT when patients have positive FDG uptake. The decision to perform FDG-PET/CT should be based on "personalized medicine criteria, especially the grading, time course of the disease, speed of progression, total tumor mass, and other criteria."