A 17-year Swiss study involving pregnant women with suspected pulmonary embolism (PE) has shown that CT pulmonary angiography (CTPA) rarely indicates the disease and more often detects alternative diagnoses. Also, the radiation dose exposure dropped by one-third during the study period.
The investigation included all pregnant women referred for CTPA due to clinically suspected PE at Lausanne University Hospital in Lausanne, Switzerland. Only 7% of patients had PE and 30.1% had an alternative diagnosis, according to a team led by Dr. David Rotzinger at the department of diagnostic and interventional radiology, emergency radiology division (European Radiology, 14 November 2019).
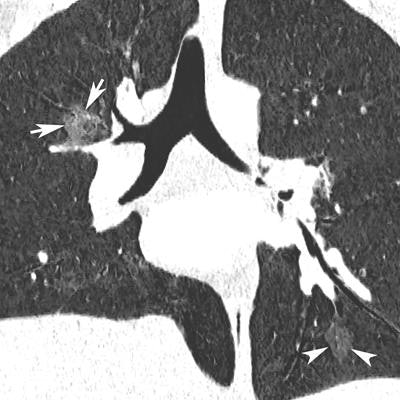
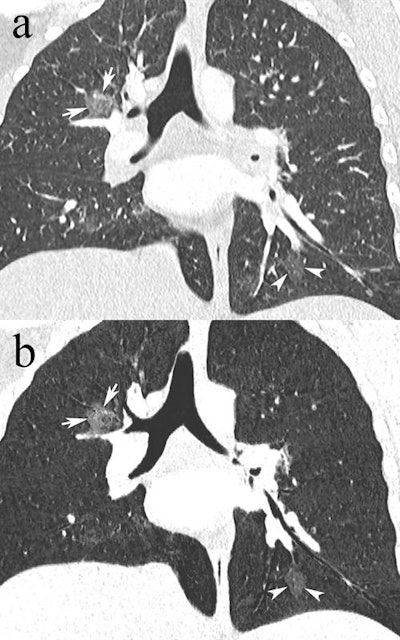 Coronal reformatted CTPA in a 23-year-old pregnant woman presenting with dyspnea and desaturation. Images in lung window (a) showed multifocal pulmonary ground-glass opacities in the right upper lobe (white arrows) and left lower lobe (white arrowheads), better depicted on minimum-intensity projection (b), consistent with viral pneumonia. The nasal swab was positive for influenza type A. Image courtesy of Drs. David Rotzinger and Sabine Schmidt.
Coronal reformatted CTPA in a 23-year-old pregnant woman presenting with dyspnea and desaturation. Images in lung window (a) showed multifocal pulmonary ground-glass opacities in the right upper lobe (white arrows) and left lower lobe (white arrowheads), better depicted on minimum-intensity projection (b), consistent with viral pneumonia. The nasal swab was positive for influenza type A. Image courtesy of Drs. David Rotzinger and Sabine Schmidt."Our paper indicates that despite the low PE rate, CTPA is still a useful test when clinical or biological features suggest PE in pregnant women, because alternative diagnoses are frequently uncovered and influence clinical decision-making," Rotzinger and one of his co-authors, emergency radiology consultant Dr. Sabine Schmidt, told AuntMinnieEurope.com.
"On the other hand, our results underline the need to improve the clinical workup of pregnant women with PE suspicion to reduce the use of ionizing radiation in those who will likely have a normal examination," they added.
PE in pregnant women
Pregnant women are four times more likely to develop PE than the nonpregnant population due to their prothrombotic state with increased coagulation factors, decreased natural anticoagulants, and impairment of fibrinolysis, according to Rotzinger and colleagues.
PE is the leading nonobstetric cause of maternal death, occurring in 1 out of 100 pregnant women diagnosed with PE. Typical PE symptoms are nonspecific during pregnancy because normal pregnancies commonly involve dyspnea, tachycardia, and leg swelling. Because of these diagnostic difficulties, pregnant women with suspected PE require additional diagnostic imaging, particularly if compression ultrasound of the legs is negative or not indicated due to the absence of leg symptoms. CTPA is the preferred method of choice due to its prolific presence and 24-hour availability.
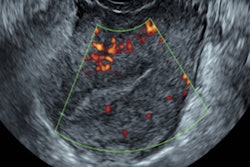
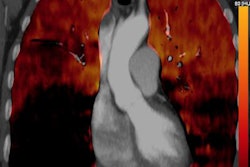
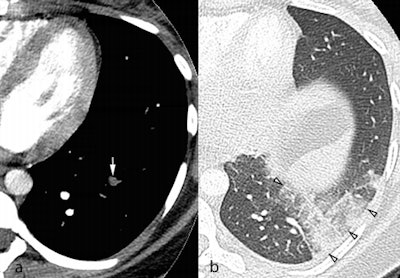 Axial CTPA images in the soft tissue (a) and lung windows (b) from a 25-year-old pregnant woman presenting with acute chest pain. A segmental pulmonary embolus was detected in the left lower lobe (a, white arrow), with associated triangular-shaped areas of subpleural alveolar density (b, arrowheads), consistent with pulmonary infarction. Image courtesy of Dr. David Rotzinger and European Radiology.
Axial CTPA images in the soft tissue (a) and lung windows (b) from a 25-year-old pregnant woman presenting with acute chest pain. A segmental pulmonary embolus was detected in the left lower lobe (a, white arrow), with associated triangular-shaped areas of subpleural alveolar density (b, arrowheads), consistent with pulmonary infarction. Image courtesy of Dr. David Rotzinger and European Radiology.Rotzinger and Schmidt said they decided to look at this topic because they noticed that in the past few years of daily work in their emergency department, more and more women entered with suspected PE, nearly always with a negative result. This piqued their interest in determining the exact results. In addition, CT is undergoing rapid technological change, leading to a reduction of radiation dose and section thickness. Would that influence image quality?
During the study period from January 2000 to August 2018, CTPA was performed using the following four CT systems:
- A 4-row MDCT system (LightSpeed QX/i, GE Healthcare) from January 2000 to November 2002; 14 examinations
- A 16-row MDCT system (LightSpeed Ultra, GE) from December 2002 to January 2006; 20 examinations
- A 64-row MDCT system (LightSpeed VCT, GE) from February 2006 to August 2015; 140 examinations
- A 256-row MDCT system (Revolution CT, GE) from September 2015 to August 2018; 63 examinations
Over time, radiation dose exposure decreased by 30%, while the number of annual examinations increased by more than fourfold, from 4.8 scans per year with the 4-row CT system to 21 scans per year with the 256-row system.
The researchers analyzed all MDCT images using a PACS workstation (Vue PACS version 11.4, Carestream Health). They visually assessed the technical quality of each CTPA using a four-point Likert scale: 0 = nondiagnostic (excluded), 1 = diagnostic image with presence of severe artifacts, 2 = good image quality with minor artifacts, and 3 = excellent image quality with no relevant artifacts. There were no significant differences among the CT systems, which had the following mean scores:
- 4-row MDCT: 2.1 ± 0.7 (n = 11)
- 16-row MDCT: 2.6 ± 0.6 (n = 20)
- 64-row MDCT: 2.5 ± 0.7 (n = 136)
- 256-row MDCT: 2.5 ± 0.7 (n = 62)
In consensus, two blinded radiologists reviewed the CTPAs of 229 patients with regard to PE, alternative diagnoses, and technical quality. The researchers found that 16 patients (7%) had PE, 144 (62.9%) had no abnormal findings, and 69 (30.1%) had an alternative diagnosis such as consolidation, other pulmonary opacities, pleural effusion, and basal atelectasis.
Among the 213 patients without PE, 35 (16.4%) had a single alternative diagnosis, while 34 (16.0%) had multiple alternative diagnoses.
"Our present study did not identify clinical and laboratory parameters that were significantly associated with PE, emphasizing the important role of CTPA for excluding PE in pregnant women," the authors wrote. "Moreover, our findings indicated a low yield of PE-positive CTPA results, which suggest the need for new diagnostic strategies to safely exclude PE with fewer radiological examinations."