In patients with early rheumatoid arthritis, using ultrasound to guide treatment doesn't produce better decision-making than the conventional treat-to-target strategy, according to a Norwegian study presented at the 2019 American College of Rheumatology/Association of Rheumatology Professionals annual meeting.
A research team from Diakonhjemmet Hospital in Oslo, led by Dr. Espen Haavardsholm, PhD, investigated whether treatment outcomes in patients with early rheumatoid arthritis can be improved by targeting imaging remission as assessed by ultrasound in addition to clinical remission. They found ultrasound failed in this regard.
"For patients, this means that if you feel that the medication has worked, your joints feel well, and your rheumatologist cannot find any signs of active joint inflammation by physical examination, there is in most cases no need to go through additional imaging exams to determine that your disease is under satisfactory control with your current medication," wrote Haavardsholm in a press release from the ACR/ARP.
Ultrasound vs. MRI
The researchers crafted a follow-up to a previous trial -- Aiming for Remission in Rheumatoid Arthritis: A Randomized Trial Examining the Benefit of Ultrasound in a Clinical Tight Control Regimen (ARCTIC), which included 230 patients with early rheumatoid arthritis who were disease-modifying antirheumatic drug (DMARD)-naïve.
They randomized the patients 1:1, with one group undergoing an ultrasound strategy targeting those with a disease activity score of less than 1.6, no swollen joints, and no power Doppler ultrasound signal in any joint. The second group received a conventional strategy that classifies patients based on a disease activity score of less than 1.6 and no swollen joints. All patients were treated by the same DMARD escalation algorithm. They started with methotrexate; then escalated to combination therapy with methotrexate, sulfasalazine, and hydroxychloroquine; and, finally, a biologic DMARD.
"The purpose of this follow-up study was to use MRI, which is reliable, objective, and more sensitive than x-ray, to make a secondary assessment of inflammatory activity and structural damage progression in the two study arms," Haavardsholm wrote in the press release. "If there really were a difference, we would expect to see it in the MRI results."
In the ultrasound arm, physicians stepped up treatment if indicated by the ultrasound score, overruling the disease activity score and swollen joint count. MRI of the dominant hand was performed six times and scored in chronological order by a blinded reader. After exclusions, 218 patients (ultrasound n = 116, conventional n = 102) had MRI at baseline and at one or more follow-up visits.
A combined inflammation score was computed by normalized summation of the synovitis, tenosynovitis, and bone marrow edema scores. A combined damage score was computed by normalized summation of the erosion and joint space narrowing scores.
The proportion of patients in each treatment arm with MRI erosive progression after two years was calculated, using the smallest detectable change (0.61) as the cutoff.
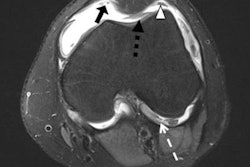
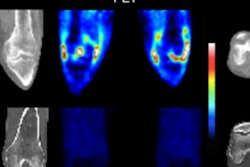
 MR images of the wrist at baseline and three-month follow-up, pre- and postgadolinium (Gd), show reduction of synovitis and tenosynovitis. Images are from Diakonhjemmet Hospital and not an actual patient in ARCTIC. Images courtesy of Dr. Espen Haavardsholm.
MR images of the wrist at baseline and three-month follow-up, pre- and postgadolinium (Gd), show reduction of synovitis and tenosynovitis. Images are from Diakonhjemmet Hospital and not an actual patient in ARCTIC. Images courtesy of Dr. Espen Haavardsholm.Nix ultrasound
The researchers found no statistically significant baseline differences between the two treatment groups in either of the combined MRI scores. The mean combined MRI inflammation score decreased during the first year in the ultrasound group by 64.2 and in the conventional strategy group by 59.4. These scores were maintained at the same level throughout the second year of follow-up.
There was no significant difference in change from baseline between the two groups at any time. The mean combined MRI damage score showed a small increase over time, with no significant difference between the two groups. In the ultrasound group, 39% of patients had MRI erosive progression compared with 33% in the conventional strategy group.
"Our findings confirm the main conclusion from the ARCTIC trial that targeting ultrasound remission does not lead to improved results," Haavardsholm wrote. "The main message is that people with rheumatoid arthritis should be diagnosed and started on treatment early, monitored closely, and treatment should be stepped up aggressively until the target of clinical remission is reached. This strategy has proven very successful. However, going beyond this by aiming to also achieve imaging remission increases treatment cost and effort, but does not significantly further improve the results."