What are the key indications, advantages, and limitations of postmortem pediatric imaging? And what is the role of 3D printing in this area? Dr. Owen Arthurs, a consultant pediatric radiologist at London's Great Ormond Street (GOS) Hospital and associate professor of radiology at the University College London GOS Institute of Child Health, provides some answers. Below is an edited version of the British Institute of Radiology (BIR) podcast on this topic, posted on 3 May. The interviewer was Miranda Wilson-Wood, content development manager of the BIR.
Wilson-Wood: Please could you tell us a bit more about postmortem imaging and children. Why do parents prefer it to conventional autopsy?
Arthurs: Autopsy is the best way to find out why a baby or a child has died. We know that both clinicians and parents are quite keen to have answers when something like that has happened, but we also know that parents aren't really very keen on incisions to the baby, as a traditional autopsy involves. We've developed a way of offering parents answers to why their baby may have died without using incisions, using imaging as an alternative. We have a variety of different imaging techniques we can offer, and they help us to decide whether or not any more investigations are needed or whether or not we've got enough information to let parents know.
What are the key indications, advantages, and limitations of postmortem imaging?
The main indications to use imaging are when parents don't want an invasive autopsy, but we can offer imaging for all kinds of perinatal and neonatal deaths, including miscarriages, stillbirths, and confirming congenital abnormalities following termination of pregnancy. We try to use the right imaging for the right indication. For example, if we have a baby whom we think may have died from skeletal dysplasia, an x-ray might give us all the answers that we need to then proceed to genetic testing. In congenital heart disease and intracranial abnormalities, it is much more appropriate to use postmortem MRI, while in cases of rib fractures in suspected physical abuse, it is best to use CT.
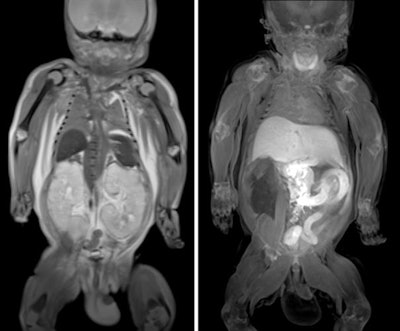 Body postmortem fetal MRI. Coronal T2-weighted (left) and T1-weighted (right) images from a 33-week fetus with autosomal recessive polycystic kidney disease and pulmonary hypoplasia. T2-weighted images demonstrated the enlarged kidneys and hypoplastic lungs (left), and T1-weighted images showed the normal high T1-weighted signal in the thyroid, meconium in the colon, and high T1-weighted signal in the liver (right). Courtesy of Norman W et al. Perinatal and pediatric postmortem magnetic resonance imaging (PMMR): sequences and technique. Br J Radiol. 2016;89(1062). doi:10.1259/bjr.20151028.
Body postmortem fetal MRI. Coronal T2-weighted (left) and T1-weighted (right) images from a 33-week fetus with autosomal recessive polycystic kidney disease and pulmonary hypoplasia. T2-weighted images demonstrated the enlarged kidneys and hypoplastic lungs (left), and T1-weighted images showed the normal high T1-weighted signal in the thyroid, meconium in the colon, and high T1-weighted signal in the liver (right). Courtesy of Norman W et al. Perinatal and pediatric postmortem magnetic resonance imaging (PMMR): sequences and technique. Br J Radiol. 2016;89(1062). doi:10.1259/bjr.20151028.More recently, we've developed micro-CT, which is a new technique to look for abnormalities in very, very small fetuses and we're developing that for fetuses lost in early pregnancy. It means early miscarriages around 12 to 16 weeks' gestation can be diagnosed, which wasn't possible with normal clinical imaging techniques.
There are some limitations to postmortem imaging in general, e.g., lung imaging still isn't very good, yet quite a lot of children may die of chest infections and lung infections, which might therefore still involve taking a tissue sample from the lung. That's part of a research project that we have going on.
How can postmortem imaging be used in medicolegal cases, for example, in cases of suspected child abuse and nonaccidental trauma?
Suspected physical abuse is commoner than you think in the U.K. and elsewhere, and imaging is a key part of making the diagnosis. Death will occur as a result of some of the most severe abuse cases, due to the injuries, and we use postmortem imaging in that setting to detect some of the injuries that a child may have suffered, such as intracranial injuries, skull fractures, and fractures in the body. We've recently shown that CT is particularly good at detecting rib fractures and subtle abnormalities elsewhere in the body that might not be detected with other imaging modalities.
3D printing techniques can be an advantage in legal cases, and we can now print out 3D models to help parents, the police, and the courts and even juries to explain quite what has happened to the child in that setting.
Overall, 3D printing is now a fairly cheap and reproducible way of showing imaging data in a simple and easily understandable way. We use 3D printing within our institution mainly for educational purposes (see figure). We have printed a femur with a bone abnormality and a skull with a fracture to show parents and others what these look like.
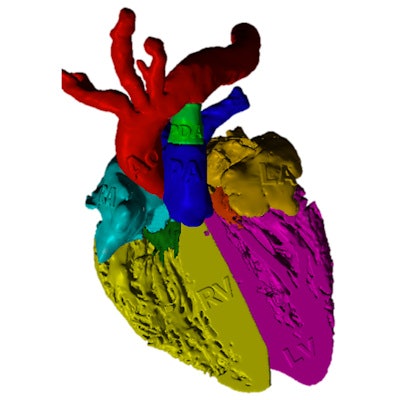
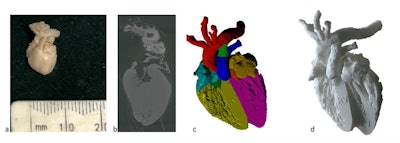 3D printing from micro-CT of a 16-week gestation fetal heart. (a) External appearances of the fetal heart, measuring less than 1 cm in length; (c) virtual 3D volume-rendered micro-CT imaged model with cardiac segments color coded. The final 3D-printed model (d) was resized to 10 x 10 x 10 of the original dimensions for use as an educational tool. Courtesy of Shelmerdine SC et al. 3D printing from microfocus computed tomography (micro-CT) in human specimens: education and future implications. Br J Radiol. 2018;91(1088). doi:10.1259/bjr.20180306.
3D printing from micro-CT of a 16-week gestation fetal heart. (a) External appearances of the fetal heart, measuring less than 1 cm in length; (c) virtual 3D volume-rendered micro-CT imaged model with cardiac segments color coded. The final 3D-printed model (d) was resized to 10 x 10 x 10 of the original dimensions for use as an educational tool. Courtesy of Shelmerdine SC et al. 3D printing from microfocus computed tomography (micro-CT) in human specimens: education and future implications. Br J Radiol. 2018;91(1088). doi:10.1259/bjr.20180306.I think we will use 3D printing much more as an educational tool in the future, particularly in teaching anatomy to medical students. The main limitations are the cost of printing, which is coming down all the time (based on the material you choose to print, it is currently around 10 to 50 pounds [11 to 57 euros] per case) and the time it takes to print; a detailed model with high resolution can take several hours to print. These factors are likely to improve with increasing use and accessibility.
We are currently undertaking a study to look at how parents would like to receive this type of information from a postmortem, and 3D printouts may play an important role in that.
Can you tell us more about the findings on postmortem imaging? For example, what are the most common pathological items seen?
In postmortem imaging, quite a lot of findings will be normal, but that can still be reassuring for parents who want to know whether or not, for example, there may have been a problem with the child or with the baby or with the placenta, or whether it was just something that happened in pregnancy. Doing a whole-body MRI of the baby after it has died and showing parents that everything is normal can be quite reassuring.
Otherwise, we need to look out for common congenital abnormalities, where the heart, brain, or kidneys, for example, haven't developed properly and have probably contributed to the death. In older children, we often pick up on infections as the cause of death, and some have died from a known cancer and we're able to identify the extent of those.
Most parents really want to get involved in autopsy and imaging techniques. They really want to know the information about why the baby or child has died. They're very keen to contribute to research, and quite a lot of studies have shown that being involved in this process helps hugely with coping and well-being and future psychological health, as well as developing the policies and practices around how we do this in future. Most of them dislike the idea of an invasive autopsy, particularly the issues around organ retention and communication and the understanding of what's going to happen. We didn't find that religious or cultural views played a big part; we found that most of those themes were common across many different religions.
What do you see for the future of postmortem imaging and pediatric patients, say, in the next five to 10 years?
I think we're still at the beginning. We've probably worked for five or 10 years to develop postmortem imaging to a point where it works now, so the next five or 10 years will be spent developing this service to provide this for all patients. We've established international working groups of radiologists and pathologists to help work together to common standards. In the U.K. National Health Service, there's currently a little bit of a postcode lottery about what you get offered around the country. Our challenge is to push this forward and to bring it into mainstream practice. Parents and support groups are very keen for this to be made available to all parents, or at least the choice to be made available so that they can choose what's best for them, and we'd like to help parents as much we as possibly can in this way.



















