An upgrade to a proven MRI method for measuring certain brain regions may help differentiate Parkinson's disease from progressive supranuclear palsy (PSP) with parkinsonism, according to researchers from Italy. Results of their study were published online on 13 February in Movement Disorders.
The MR Parkinsonism Index (MRPI) has been used to diagnose patients with suspected PSP, but its method of calculation has achieved subpar sensitivity in distinguishing between PSP-parkinsonism and Parkinson's disease. By adding another factor -- measurement of the brain's third ventricle -- to create the MRPI 2.0, the researchers found a better way to distinguish between the maladies and to predict which patients could develop future conditions such as vertical gaze abnormality (VGA).
"Our findings demonstrate the usefulness of these new imaging biomarkers, and specifically of the MRPI 2.0, in predicting the development of VGA and the clinical evolution toward PSP phenotypes in patients with the initial diagnosis of Parkinson's disease," wrote the group led by Dr. Aldo Quattrone from the Neuroscience Centre at Magna Graecia University in Catanzaro. "These biomarkers could help clinicians identify very early those patients who may change the initial diagnosis from Parkinson's to PSP-parkinsonism, thus impacting on patient counseling, prognosis, and therapeutic strategies."
Diagnostic challenge
Accurately diagnosing Parkinson's disease is challenging, especially in its early stages because the typical clinical indications of the disease are not yet fully present. The most frequent misdiagnoses involve atypical parkinsonisms, which include multiple system atrophy or progressive supranuclear palsy. Recent studies have shown that differentiating Parkinson's disease from PSP with parkinsonism is an even greater challenge.
"The clinical presentation of PSP-parkinsonism resembles idiopathic Parkinson's disease to such an extent that the two disorders are difficult to distinguish early on," the authors wrote.
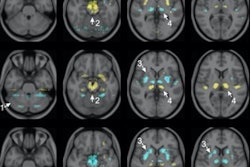
Clinicians have used the MRPI to measure the width of the superior and middle cerebellar peduncles and the area of the midbrain and pons, and this approach has been shown to predict which patients might progress to PSP-parkinsonism and possibly develop vertical gaze abnormalities. However, the MRPI has achieved low sensitivity in differentiating PSP-parkinsonism patients from individuals with Parkinson's disease.
To solve that problem, Quattrone and colleagues created the MRPI 2.0. Their upgrade adds the width of the third ventricle, one of four connected fluid-filled cavities in the brain's ventricular system, to existing calculations. So far, the modification has worked well. In a 2018 study by Quattrone et al, the MRPI 2.0 achieved sensitivity of 100% and specificity of 94% in differentiating PSP-parkinsonism from Parkinson's disease (Parkinsonism & Related Disorders, September 2018, Vol. 54, pp. 3-8).
In the current prospective study, the Italian researchers tested the capabilities of the MRPI 2.0 by following patients with an initial clinical diagnosis of Parkinson's for four years to see if they could determine which patients actually had PSP-parkinsonism, based, in part, on the presence of vertical gaze abnormalities.
"VGA usually are the most specific neurological signs for differentiating patients with PSP-parkinsonism from those with Parkinson's disease; however, these clinical features may occur later or never in PSP-parkinsonism patients," the group wrote. "The absence of VGA makes it difficult to differentiate between patients with PSP-parkinsonism and those with Parkinson's disease, suggesting that the true prevalence of PSP-parkinsonism may be underestimated."
The researchers consecutively recruited 110 patients with Parkinson's, along with 74 healthy control participants who matched for age and gender. All of the subjects underwent brain MRI scans on a 3-tesla system (Discovery MR750, GE Healthcare) with an eight-channel head coil. The researchers also performed automated measurements to calculate the pons/midbrain area ratio (P/M) and the MRPI, before adding the third ventricle measurement to upgrade to P/M 2.0 and MRPI 2.0.
Further verification
At the four-year follow-up, the initial diagnosis of Parkinson's was confirmed clinically in 100 patients (91%), while the other 10 patients (9%) had their diagnosis changed from Parkinson's to PSP-parkinsonism with signs of vertical gaze abnormality. At follow-up, the P/M 2.0, MRPI, and MRPI 2.0 all accurately distinguished the 10 patients with PSP-parkinsonism from those with Parkinson's disease.
There was, however, one significant difference between the three approaches. At baseline, only the MRPI 2.0 predicted the development of VGA in all 10 patients to achieve 100% sensitivity and specificity. It was not until the end of the four-year follow-up that the other two imaging biomarkers accurately differentiated PSP-parkinsonism patients from those with Parkinson's.
"In Parkinson's disease patients, baseline Magnetic Resonance Parkinsonism Index 2.0 showed the best performance in predicting the clinical evolution toward a PSP-parkinsonism phenotype, enabling PSP-parkinsonism patients to be identified at the earliest stage of the disease for promising disease-modifying therapies," Quattrone and colleagues concluded.