Researchers from Dublin have described precisely how to optimize CT protocols for detecting injuries to the renal parenchyma, vasculature, and collecting system, and they have also elaborated on CT findings and management options for each grade of injury.
"Radiology plays a central role in the management of renal trauma, both from a diagnostic and therapeutic viewpoint," noted Dr. Marie Bambrick and colleagues at St. James's Hospital. "Accurate evaluation of renal injuries on CT can often allow a nonoperative approach and improve patient outcome. Detection and accurate grading of injuries on the imaging findings is, therefore, of critical importance."
Renal injury occurs in about 5% of all trauma cases and 10% of abdominal trauma patients; in most cases, the renal injury results from blunt trauma (90%), with penetrating injuries accounting for only 10% of cases, they explained.
The mechanism of injury in blunt trauma can be due to direct impact or rapid deceleration, such as in road traffic accidents (RTAs) or a fall from a height. While road accidents usually result in injury to the renal parenchyma (contusions, hematomas, and lacerations), a fall from a height can cause injury at the renal pedicle, where it is more mobile within the abdominal cavity.
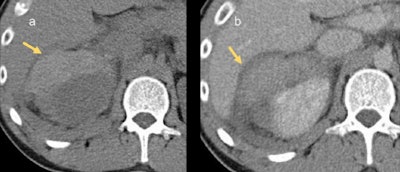
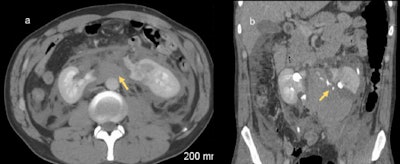 A 33-year-old man following a road traffic accident. There is fragmentation of a horseshoe kidney with a large retroperitoneal hematoma (a) and extravasation of contrast-enhanced urine from the collecting system indicating collecting system injury (b). Horseshoe kidneys are more vulnerable to injury in blunt abdominal trauma due to their position anterior to the spinal column. All images courtesy of Dr. Marie Bambrick. © Radiology Department, St James's Hospital, Dublin.
A 33-year-old man following a road traffic accident. There is fragmentation of a horseshoe kidney with a large retroperitoneal hematoma (a) and extravasation of contrast-enhanced urine from the collecting system indicating collecting system injury (b). Horseshoe kidneys are more vulnerable to injury in blunt abdominal trauma due to their position anterior to the spinal column. All images courtesy of Dr. Marie Bambrick. © Radiology Department, St James's Hospital, Dublin."Renal trauma is more severe in patients with underlying renal abnormalities, both congenital and acquired, for example horseshoe kidney, cross-fused ectopia, pelvic kidney, or hydronephrosis. In these patients, the assessment of renal injury on imaging can also be more challenging," Bambrick told delegates at ECR 2018.
Think conservative
Because surgical exploration for renal trauma has a high nephrectomy rate, it is commonly accepted that a conservative approach to management is preferable when possible, Bambrick continued. The following four steps are essential:
- Accurately stage the injury.
- Identify pre-existing renal pathology.
- Document the function/presence of the uninjured kidney.
- Identify injuries to other intra-abdominal organs.
Modalities other than CT have only a limited role in the imaging of acute renal trauma. A focused abdominal sonography in trauma (FAST) scan in the emergency department can be useful for identifying free intra-abdominal fluid, but it does not adequately assess the retroperitoneum and is not sensitive at detecting vascular injuries, according to the researchers. MRI is generally not practicable in acute trauma cases, but it may be used for follow-up.
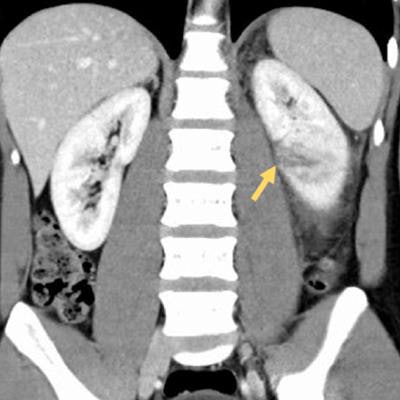
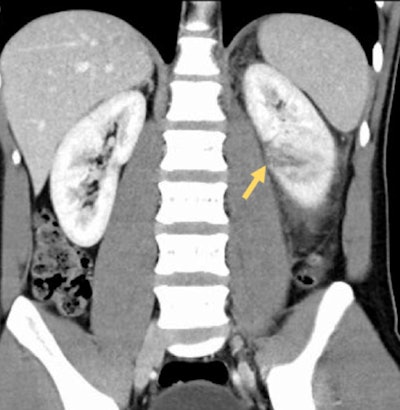 A 46-year-old man post blunt trauma following assault. A linear focus of low attenuation is visible in the lower pole of the left kidney, representing a grade III laceration.
A 46-year-old man post blunt trauma following assault. A linear focus of low attenuation is visible in the lower pole of the left kidney, representing a grade III laceration.They urged everyone to get to know the CT renal trauma guidelines of the European Association of Urology and the American Urological Association, which broadly agree and can be summarized as follows:
- Hemodynamically unstable patients should be brought directly to the operating room for exploratory laparotomy.
- Stable patients who have undergone blunt abdominal trauma and have either gross hematuria or microscopic hematuria, as well as evidence of shock (i.e., systolic blood pressure [SBP] < 90 mm Hg), should undergo contrast-enhanced CT.
- Stable patients who have undergone blunt abdominal trauma and have microscopic hematuria only -- with nothing else to suggest renal injury -- do not require imaging.
- Patients who have undergone trauma in which the mechanism of injury raises a suspicion of renal injury (e.g., rapid deceleration, significant blow to flank, penetrating trauma, extensive bruising over flank, or rib fracture) should undergo contrast-enhanced CT.
If the mechanism of injury or clinical picture indicates significant injury, the absence of hematuria should not act as a barrier to imaging because hematuria is only present in a minority of renal trauma cases and does not correlate with severity of the injury, the researchers stated.
 This 52-year-old man involved in a road traffic accident has a right perinephric hematoma. The irregular area of free fluid is hyperattenuating on the noncontrast study (a), indicating it is an acute hematoma.
This 52-year-old man involved in a road traffic accident has a right perinephric hematoma. The irregular area of free fluid is hyperattenuating on the noncontrast study (a), indicating it is an acute hematoma.Imaging protocol
In cases of renal trauma, the imaging protocol used should adequately assess three key components of the kidney: the parenchyma, vasculature, and collecting system.
"Imaging usually occurs in the setting of general abdominal trauma for which a trauma protocol is employed to assess for a wide range of injuries," Bambrick and colleagues continued. "A trauma protocol for the abdomen involves portal venous-phase imaging, which corresponds with the corticomedullary phase, thus enabling assessment of renal parenchyma. There is also an increasing tendency to include an arterial phase in the trauma protocol to assess for arterial injury."
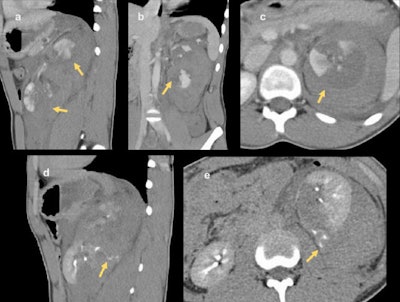 Shattered kidney in 16-year-old boy following blunt trauma in a sports match. The left kidney is divided in two (a) and (b). Extensive areas of nonattenuating parenchyma are visible in the upper pole (c) in keeping with devitalized fragments. On delayed-phase
Shattered kidney in 16-year-old boy following blunt trauma in a sports match. The left kidney is divided in two (a) and (b). Extensive areas of nonattenuating parenchyma are visible in the upper pole (c) in keeping with devitalized fragments. On delayed-phaseimaging (d) and (e), extravasation of contrast material from the collecting system of the lower pole can be seen. This patient subsequently underwent left nephrectomy.
In cases of penetrating trauma, preliminary noncontrast CT images may be of benefit in identifying and distinguishing extravasation from foreign bodies. If there is suspicion of an injury to the collecting system based on the initial scan, a delayed or excretory phase should be performed after 10 to 20 minutes. Injuries to the collecting system may be indicated on the initial scan by evidence of a laceration that appears to extend to the collecting system or by the presence of perinephric free fluid. Delayed-phase images also are useful in evaluating vascular injuries, such as active bleeding and pseudoaneurysm, the researchers noted.
The American Association for the Surgery of Trauma (AAST) has developed a scale (grades I-V) for classifying renal injury in the setting of trauma, and this scale is widely used to grade the severity of renal injury and is helpful in planning patient management.
"It is vital that an appropriate CT protocol is used when assessing these patients and that the radiologist is familiar with the AAST grading system and the implications for patient management," they concluded. "Of particular importance is an understanding of how to assess for collecting system injury."
The group's e-poster presented at ECR 2018 received a certificate of merit award, and it is accessible via the ESR website.